“High Calcium Food Chart” is written by Arantza Barroso, RDN. Updated by Katie Dodd, MS, RDN, CSG, LD, FAND.
Calcium is the key to keeping strong bones and preventing osteoporosis as we age. But, did you know that calcium is used by almost every organ in the body?
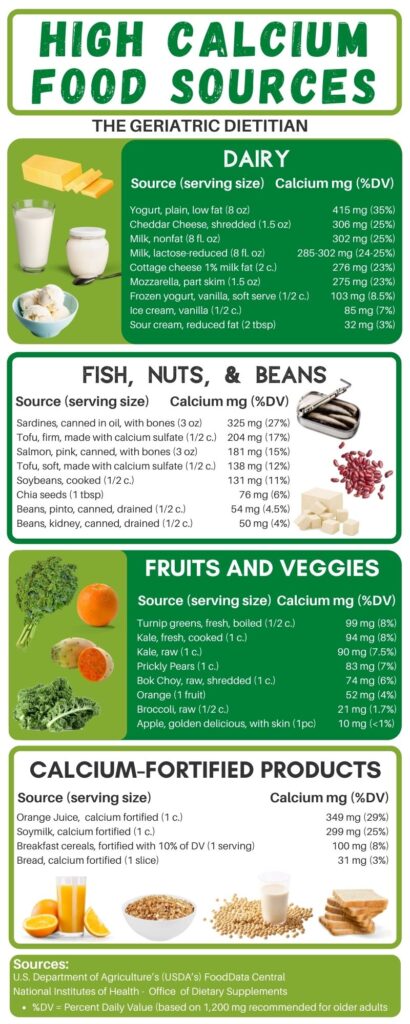
Keep reading to see how to include calcium in your diet! And to check out our high calcium food chart with 29 delicious high calcium foods.
High Calcium Food Chart
This high calcium food chart groups foods into different categories. And it includes the amount of calcium per serving and % daily value based on the 1,200 mg calcium recommendation for older adults.
Why is calcium important?
Calcium is the #1 mineral in the body! Calcium makes up 39% of the minerals in the body. And almost every cell in the body uses calcium to work correctly.
It helps your heart to beat. And it helps your muscles move. It helps to control hormones, helps blood to clot, and optimizes brain function.
The organs in the body constantly use calcium. However, most of the calcium that is present in the body is stored in the bones and teeth (like 99%!). Therefore, it is important to keep them strong as we age.
The body recycles calcium as needed for all of the different cells to function right. Therefore, we must try to maintain optimum calcium levels. So that it is not constantly being taken away from the bones.
Calcium and bone health
Calcium plays a role in many health conditions. But it is especially important for bone health in older adults.
The structure of bones is made up mostly of calcium. And the bones act as a form of calcium reservoir that helps keep balanced levels of calcium in the body.
To do this, the bones go through a constant remodeling cycle- breaking down to release calcium and rebuilding the bone by storing more calcium that comes from the diet.
This is a crucial process for proper bone growth and calcium maintenance as we age.
Every day the body loses calcium through the skin, nails, hair, sweat, and urine.
Since the body cannot produce calcium (it can only recycle it), it is very important to replenish the calcium that is lost. We do this by eating foods high in calcium to preserve strong and healthy bones. (5)

Calcium Deficiency
Calcium deficiency can cause the bones to become fragile and soft.
This can be a significant problem for older adults. Older adults often have a higher risk of falls and fractures. As such, falls may cause other health complications.
Potential causes of calcium deficiency:
- Not eating enough high calcium foods
- Deficiencies of other nutrients like vitamin D and magnesium
- Underlying conditions such as hypothyroidism
- Postmenopausal women
- Critical illnesses
- Using certain medications that impair calcium absorption
- Etc.
Usually there are no apparent symptoms of a calcium deficiency. Especially when calcium levels are mildly low.
However, since calcium is involved in so many different body functions, the symptoms occur in more severe deficiencies.
Symptoms of calcium deficiency may include:
- muscular numbness
- tingling in the hands and feet
- muscle spasms
- depression
- confusion
- seizures
- abnormal heart rhythms
- or even a coma in rare cases
It is very important to talk to your doctor if you are concerned about being deficient in calcium. We want to correct a deficiency early enough to avoid further complications.
Who is at Risk for Calcium Deficiency?
The groups of people who are most likely to have a calcium deficiency are postmenopausal women and those who follow a dairy free diet.
Postmenopausal women
After menopause, there is significant bone loss in women. This is because of a decrease in estrogen production in the body.
Estrogen is involved in calcium absorption. And the lack of estrogen production after menopause increases the amount of calcium that is lost through the urine.
When calcium is lost through the urine, more calcium is taken from the bones.
Over time, the bones will continue to break down to allow calcium to be used for other things. And not enough calcium will be restored back in the bones, causing them to become weaker and softer.
Postmenopausal women are losing about 1% of their bone mass every single year. And 30% end up developing osteoporosis (1).
It is very important for aging women to get enough calcium in their diets.
Dairy Free Diet
Individuals may follow a dairy free diet for many reasons: personal preference, being lactose intolerant, being allergic to milk, or following a vegan diet.
Dairy products typically contain the highest amounts of calcium. Therefore, following a dairy-free diet increases the risk of being calcium deficient. However, this can be avoided by eating plenty of plant-based calcium sources.
Lactose-free dairy is still a good source of calcium for those who are lactose-intolerant that choose to consume dairy.
Another option for a dairy-free diet is to consume foods that are fortified with calcium such as orange juice, bread, and cereals.
Factors influencing calcium absorption
There are several factors that affect how much calcium is absorbed by the body.
These factors include:
- Vitamin D
- Vitamin D is necessary to absorb calcium and regulate your calcium levels. Low levels of vitamin D can significantly decrease the amount of calcium the body absorbs.
- Age
- The body naturally cannot absorb as much calcium as we age.
- Hormonal status (estrogen levels)
- A decrease in estrogen levels is related to decreased calcium absorption and increased risk of osteoporosis in women.
- Interactions between calcium and other nutrients
- Some nutrients can interfere with calcium use. These include oxalate, phytate, and fiber (in large amounts).
- Other nutrients help calcium absorption.
Foods that help the body use calcium
Foods that interfere with the body using calcium
Certain compounds in plants can decrease the amount of calcium absorption. This is because these compounds can interact with the dietary calcium. And block it from being used by the bones.
The main nutrients that interfere with calcium are:
- Oxalic Acid (oxalate)
- Found mostly in leafy greens: spinach, collard greens, sweet potato, rhubarb
- Interferes with calcium absorption
- Phytic Acid (phytate)
- Found mostly in bran and seeds
- Interferes with calcium absorption
- Fiber (in large amounts)
- Found in whole grains, fruits, and vegetables
- Excessive amounts of fiber can decrease calcium absorption
Spinach is actually a high calcium food source. However, it is also high in oxalic acid. This means the body is not able to use all of that good calcium.
It is estimated that only 5% of the calcium in spinach is actually absorbed and used by the body. This is why you will not see spinach listed in our high calcium food chart.
When many different sources of calcium (dairy and plant-based) are included in the diet, the interactions between calcium and these compounds are not as significant. So do not worry too much!
You can still eat your spinach. Just make sure you get other good sources of calcium throughout the day.
Foods that cause calcium to be excreted from the body
These compounds do not necessarily affect calcium levels to a high extent. However, eating high amounts of these foods could have a greater consequence if there is a calcium deficiency.
Dietary sodium (salt) influences the amount of calcium that is lost through the urine. This is especially important to consider for older women. Because losing too much calcium and consuming too much salt can cause the bones to weaken much faster (6).
Phosphorous and caffeine may also have a negative impact on calcium levels. Especially when consumed in large doses. However, we need more research. (6).

Osteoporosis
Osteoporosis is a skeletal disease. Bone density becomes very low. And the bones become weaker and softer, which results in a high risk of fractures.
Bones go through a remodeling process so that calcium can be used throughout the body.
But as we age, the ratio of bone dissolving and rebuilding changes. And more bone tissue is lost than rebuilt.
When the body doesn’t get enough calcium, the bones break down to recycle the calcium that is stored. Because your body needs that calcium to function! As a result, the bones become more and more fragile.
Osteoporosis is a “silent disease.” This means that there are no visible symptoms. That is, until a fracture occurs and it typically affects older adults.
Postmenopausal women are especially at risk of developing osteoporosis. Because of the hormonal changes that happen in the female body.
It is very important for older adults to talk to their doctors or healthcare providers about the possibility of developing osteoporosis. And to get screened for osteoporosis early.
Early diagnosis can help prevent the bones from becoming too fragile. And to avoid fractures that could significantly impact the quality of life of older adults.
Risk of fractures
Fractures can happen unexpectedly to older adults who are diagnosed with osteoporosis.
These fractures are most common on the hips, the wrists, and spinal vertebrae (the back!), and can unfortunately be caused by minor falls or even normal everyday movements.
However, it is possible to manage osteoporosis and prevent fragility fractures by increasing levels of calcium, vitamin D, and exercising consistently.
Preventing falls and fractures is important to preserve the independence of older adults and delay disability as much as possible.
Learn more information about osteoporosis in the elderly.
Calcium needs for older adults
The RDA (recommended dietary allowance) for calcium is the average daily amount of calcium we should have every day.
How much is needed to maintain bone density as we age. And to promote calcium balance in the bones.
Recommended Calcium Intakes
The calcium recommended intake for older adults (4):
- Men:
- <70 years: 1,000 mg/day
- 71+ years: 1,200 mg/day
- Women:
- 19-50 years: 1,000 mg/day
- 51+ years: 1,200 mg/day
Calcium Toxicity
While calcium is an important nutrient, too much can be a bad thing.
How much calcium is too much calcium?
Older adults should consume adequate calcium to preserve their bone health. However, there is a risk of consuming too much calcium.
Excessive levels of calcium are rare in relatively healthy people. And usually, only occur if there is an underlying condition such as cancer or thyroid malfunction.
However, it is important to note that excessive calcium can lead to several conditions. These conditions could greatly affect the health status and quality of life of older adults.
These conditions range from constipation, nausea, weight loss, and fatigue to renal failure, heart arrhythmias, and even heart attacks.
The Food and Nutrition Board established the upper levels for calcium based on many studies focusing on high calcium consumption and its effects, which included a high risk of kidney stones.
The tolerable upper intake levels for calcium as determined by the Food and Nutrition Board are the same for men and women over the age of 50. It is acceptable to consume no more than 2,000 mg of calcium per day for both men and women. (1)
Risk of Kidney Stones
Remember oxalate? Studies show that when there is excess oxalate in the urine, it can stick to calcium and form stones in the kidneys. (2)
Some factors that may increase risk of calcium-oxalate stones are eating too many calcium-rich and oxalate-rich foods, certain health conditions, eating a poor diet, etc.
However, note that cutting out all of these nutrients is dangerous and can cause other health problems. It is important to talk to your dietitian or healthcare provider about these risks and learn the best way to include all of these nutrients in your diet. (3)
Types of Calcium Sources
Calcium can come from dairy, plant-based sources, fortified foods, or supplements.
Animal Calcium Sources
Plain yogurt, milk, and cheese are very rich sources of calcium.
In case of a lactose intolerance, you can opt for lactose-free products. Lactose-free products remove the lactose (milk sugar), but still contain high amounts of calcium.
It is important to note that dairy products that are lower in fat content have the highest amounts of calcium available for the body to absorb.
Canned sardines and canned salmon are also good sources of calcium because these usually contain bones.

Plant-based Calcium Sources
Plant-based sources of calcium are good for those who don’t drink dairy. Good sources of plant-based calcium include vegetables such as broccoli, collard greens, kale, bok choy (also known as Chinese cabbage), and soybeans.
Tofu processed with calcium salt is also a great source of calcium.
Make sure you check food labels for calcium content!

The table below includes high protein calcium sources. This includes animal-based calcium sources (fish) and plant-based calcium sources. We’ll cover plant-based calcium sources next.

Fortified Calcium Sources
Many foods are fortified with calcium including fruit juices, bread, and ready-to-eat cereals.
These foods are great sources of calcium since they are food items. Especially since they are staples in many American households.

Calcium Supplements
You should get most of your daily calcium intake from food rather than supplements. To prevent health complications related to excess calcium in the body.
However, low-dose calcium supplements can fill in gaps in the diet. There are three common calcium supplements you might see at the pharmacy or health stores.
Types of calcium supplements:
- Calcium citrate
- Calcium ascorbate
- and Calcium carbonate
Low-dosage supplements (supplements that contain less than 500mg of calcium per serving) are safer to consume to avoid causing any damage to the body.
Some supplements may cause gastrointestinal side effects in older adults like gas, constipation, and/or bloating.
Talk to your doctor to determine if a calcium supplement is right for you!
How to include calcium in your diet
Here are some tips to get the most calcium from your food:
- Try adding at least one calcium-rich food from the high calcium food chart in your meals and snacks throughout the day.
- Use low fat or 1% milk for your morning smoothie or oatmeal.
- You can also add kale in your smoothies. I promise your smoothie will not taste like kale! The fruit will cover the taste and you will have a delicious calcium-rich meal.
- Include string cheese (mozzarella and cheddar are high in calcium) as an easy snack on the go.
- Canned sardines or pink salmon is a great snack to serve with crackers.
- Use fortified soymilk as a great plant-based option in any recipe with milk.
- Craving sweets? Instant chocolate pudding uses dried milk powder which is high in calcium! This is a great sweet option to satisfy your sweet tooth.
Conclusion – High Calcium Food Chart
Calcium has many vital functions and it is very easy to overlook our daily calcium intake. Here are the key things to remember:
- It is important for older adults to include high-calcium foods in every meal to maintain healthy bones and avoid the risk of fractures.
- There are many types of high-calcium foods that can fit various lifestyles (dairy-free, lactose-free, etc.)
- Certain compounds affect how much calcium can be absorbed by the body.
- Too much calcium can have serious side effects that can negatively affect the quality of life of older adults.
- Refer to our high calcium food chart for good high calcium food sources!

References
- U.S. Department of Health and Human Services. (n.d.). Office of dietary supplements – Calcium. NIH Office of Dietary Supplements. Retrieved September 10, 2021, from https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/#en1.
- Massey, L. K., Roman-Smith, H., & Sutton, R. A. L. (1993). Effect of dietary oxalate and calcium on urinary oxalate and risk of formation of calcium oxalate kidney stones. Journal of the American Dietetic Association, 93(8), 901–906. https://doi.org/10.1016/0002-8223(93)91530-4
- Calcium oxalate stones. National Kidney Foundation. (2021, July 26). Retrieved September 10, 2021, from https://www.kidney.org/atoz/content/calcium-oxalate-stone.
- Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press; 2011.
- Nieves, J. W. (2003). Calcium, vitamin d, and nutrition in elderly adults. Clinics in Geriatric Medicine, 19(2), 321–335. https://doi.org/10.1016/s0749-0690(02)00073-3
- Calcium. Linus Pauling Institute. (2021, January 1). Retrieved September 10, 2021, from https://lpi.oregonstate.edu/mic/minerals/calcium.
