Failure to Thrive Elderly: Symptoms and Solutions
Failure to Thrive: Elderly was written by dietetic intern Dalia Richmond & reviewed/edited by Katie Dodd, MS, RDN, CSG, LD, FAND.
We often see failure to thrive (FTT) as a major concern for children. While failure to thrive is no less important in older adults, it can often be overlooked.
This article aims to shine a light on adult failure to thrive, and offer solutions for its signs and symptoms.
What is Failure to Thrive?
Failure to thrive is not a disease, or disorder. Rather, it is a group of signs and symptoms that lead to a higher risk of mortality, and morbidity in older patients. FTT may also decrease an individual’s quality of life.
This article will discuss how adult failure to thrive is diagnosed. We will go into depth on the symptoms and solutions (including nutrition!). And finally, you’ll learn the importance of having a registered dietitian (RD) on the healthcare team to improve outcomes and quality of life.
Diagnosis of Failure to Thrive in the Elderly
An article published in the Journal of the American Family Physician goes into depth about the initial evaluation of failure to thrive in the elderly.
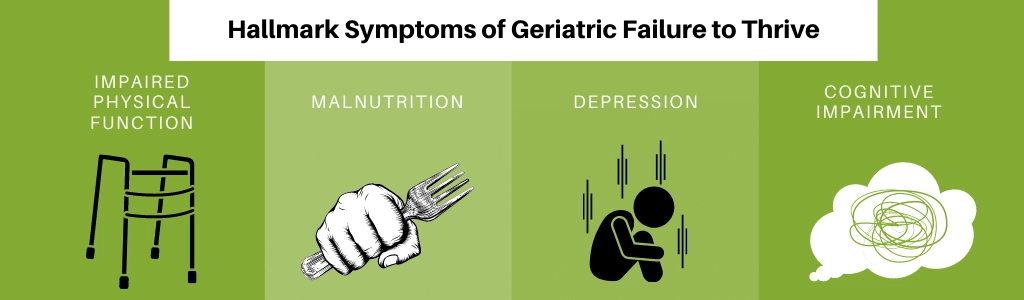
The four main symptoms associated with failure to thrive include1:
- Impaired physical function
- Malnutrition
- Depression
- Cognitive impairment
Who Can Diagnose Failure to Thrive?
Failure to thrive is diagnosed by a physician. The physician performs a thorough physical exam and obtains a history of the patient’s health.
Other medical professionals may also be involved. This may include a psychologist, occupational therapist, physical therapist, social worker, pharmacist, and dietitian. Everyone on the team is vital to helping diagnose and treat failure to thrive.
Let’s review some of the roles these medical professionals have in diagnosing the components of adult failure to thrive.
The psychologist assists with the assessment and treatment of depression in elderly persons with FTT. Depression is often assessed using the Geriatric Depression Scale and/or the Cornell Scale for Depression in Dementia. These forms are often completed by the physician or nurse as well.
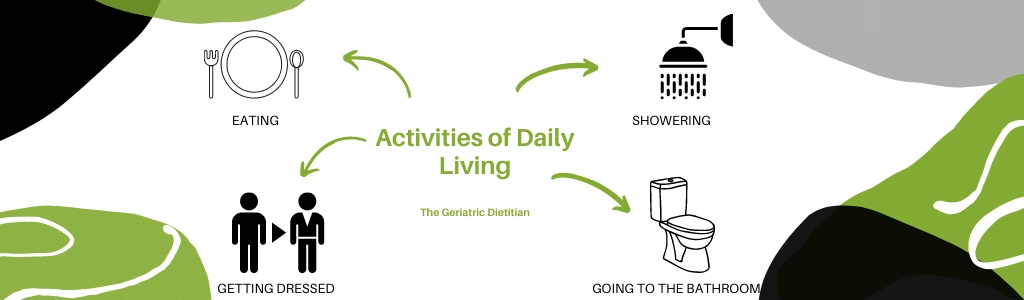
The occupational therapist (OT) assesses the patient’s ability to complete activities of daily living (ADLs). The OT can gauge what may need to be done to help increase function.
The dietitian helps with the identification of malnutrition.
Screening for Malnutrition
There are three tools that may be used to accurately screen for malnutrition. For example, the Mini Nutritional Assessment Short Form (MNA), the Malnutrition Universal Screening Tool, and the Short Nutritional Assessment Questionnaire.
All of these tools are available online to the general public, and take less than five minutes to complete. You can learn more at our article, Which Malnutrition Screening Tool is Best?
Malnutrition screening tools can be used by nurses or physicians when they first see a patient they suspect has failure to thrive. From here, they can refer the patient to a dietitian who can work with them further. The dietitian can assist in diagnosing malnutrition. And assist the patient in improving their nutrition status.
Signs and Symptoms of Failure to Thrive in the Elderly
As mentioned above, there are four main signs associated with failure to thrive.1 Let’s dig a little deeper into impaired physical function and malnutrition.
Impaired Physical Function (ADL, IADLs)
Loss of physical functional status is typically addressed by an OT, but can be identified by many members of the healthcare team. Specifically, we are looking at loss functional status in activities of daily living (ADLs) or instrumental activities of daily living (IADLs).
The NIH defines ADLs as the tasks of everyday life2, including:
- Eating
- Dressing
- Getting into or out of a bed or chair
- Taking a bath or shower
- Using the toilet
The Katz ADL Index is a helpful tool to assess independence in activities of daily living in elderly people. You can access the Katz ADL scale here: https://www.alz.org/careplanning/downloads/katz-adl.pdf.
Of note, muscle strength is important in old age to minimize functional impairments. Muscle weakness leads to physical limitations and decreased overall health.
The NIH defines IADLs as activities related to independent living2, including:
- Preparing meals
- Grocery shopping
- Managing money
- Doing housework
- Using a telephone
- Getting from one place to another (driving, walking, etc.)
Malnutrition
Malnutrition is a topic. Unfortunately, it is not noticed enough in the older adult population. One of the most defining signs of failure to thrive in both older and younger populations is weight loss and malnutrition.
A thorough nutrition assessment should be performed by a dietitian in order to determine the nutrition status of the patient. This should include a dietary intake history and a nutrition focused physical exam.
This can help the dietitian determine how much muscle wasting (loss) and fat loss the patient is experiencing. The exam may also include blood tests to look into low nutrient levels.
Treatment of Failure to Thrive in the Elderly
Treatment of failure to thrive in the elderly has many parts to it and involves many members of a healthcare team.
A Healthcare Team
Each member of the healthcare team has an important role to play in improving the health outcomes and quality of life for each patient.
Members of the healthcare team who help with FTT:
- Physician
- Nurse
- Psychiatrist
- Psychologist
- Pharmacist
- Occupational Therapist
- Physical Therapist
- Speech Therapist
- Registered Dietitian
- Etc.
The physician, psychiatrist, and pharmacist can help with medication needs. This may include SSRIs or other antidepressants. Or perhaps medications for cognitive impairment if necessary. And potentially appetite stimulants to help combat weight loss or malnutrition.1
The physician may also oversee general care, manage chronic disease, and refer the patient to other professionals.
Frequent work with an OT may be needed to address gaps in the patient’s ability to conduct ADLs or IADLs.
Malnutrition related to failure to thrive may also be related difficulty swallowing or chewing. If swallowing or chewing difficulties are noticed, the patient should be referred to a speech language pathologist (SLP). The SLP may need to perform a test to assess the patient’s ability to swallow.
The dietitian may also be applicable here to help address food access, the patient’s ability to grocery shop and cook, or the patient’s ability to eat. The dietitian often works alongside the social worker to sign the patient up for nutrition programs and discuss changes with the family.
The social worker can also help to address the social aspects of the patient’s failure to thrive. Economic status and functional ability can be indicators of nutritional status in the older adult population.
Access to Food
Some older adults may not have enough money for food. Or they simply may not be able to access food (get the food they need). Food stamp programs, Meals on Wheels, and other nutrition programs can be very beneficial for this population.
Dietitians and Social Workers generally have many resources in their local area. And programs they can refer patients or clients to when they see a need. They will have a good idea of what the patient or client needs and will work with them to find the best fitting resources.
You can learn more at our article Finding Free Meals for Seniors.
Improving Social Health
In addition to food access, social factors such as social isolation or losing loved ones due to older age or to disease, may make individuals more prone to depression or loneliness. This can then lead to decreased intake and malnutrition in older persons.
Helping to address the patient’s living situation and the potential need for assisted care may be necessary in this population.3 Referral to social worker or psychologist may be beneficial.
Why Does Malnutrition in Geriatrics Happen?
So why does malnutrition in this population happen? What research has found is that it has different parts to it.
Symptoms may include a decline in appetite associated with age or decreases in appetite related to other diseases. Signs may also include a reduction in a desire to eat due to social or economic problems, and starvation associated with depression.3
Cause of Decreased Intake
Poor appetite associated with age, often referred to as anorexia of aging, is related to changes in hormones that affect the body’s desire to eat and its ability to feel full or hungry.3
With older age and loss of muscle, how many calories a person uses daily may decrease. This can lead to a lower appetite and lower food intake. To top it all off, a decline in smell and taste may lead to less appreciation of foods and eating altogether.3
Other diseases such as cancer can lead to worsening of the symptoms above. A patient being told to follow specific diets for diabetes, kidney disease, heart disease like congestive heart failure can lead to decreased intake. Strict diets may lead to a decreased satisfaction of food due to restrictions in food groups or sodium.3
Liberalized diets for older adults are often recommended to increase intake.
As mentioned above, social and economic status as well as a patient’s ability to complete ADL’s are both problems that may lead to a poor nutrition status. If a patient cannot afford a meal, they may skip it to prioritize paying for medications or rent.
If a person cannot go grocery shopping or cook themselves a meal (IADLs) or worse, if they cannot even get out of bed due to a decrease in ADLs, the patient is unlikely to eat anything. Not only will their appetite be lower due to less physical activity, but they also may be depressed, or lack motivation to eat.
Losing family members or loved ones they once ate with (a spouse or living partner) may also lead to less desire to eat due to having to eat alone. The person may also lack motivation to prepare a meal for just one person.
A Combination of Factors
All in all, the factors that lead to malnutrition are complex. Each patient may have a different mixture of the above factors, or something that was not even mentioned.
It is important that each patient be addressed on an individual basis, and treated based on their specific health concerns.
You can learn more at Chronic Malnutrition for Seniors.
How to Improve Failure to Thrive in the Elderly
Next, let’s address how to improve failure to thrive in the elderly.
Addressing Malnutrition
Addressing malnutrition is one of the first steps to helping a geriatric patient get back on track. If the patient has malnutrition, the first step is to discover the root cause of the malnutrition.
Once the cause has been established, treatment can be started. Treatment for malnutrition may include:
- High calorie high protein diet
- Food assistance: Food stamps, Meals on Wheels, etc.
- Appetite stimulants (use with caution in elderly)
- Increased level of care: moving to an assisted living facility, having a live in caregiver, etc.
- Anti-depressants to improve depressive symptoms
- Physical or occupational therapy assistance to improve ADLs
- Regular check-ins with a Registered Dietitian
- Etc.

Protein and Calorie Needs
Nutrient and calorie needs differ in the older adult population from those in the general adult population. The following nutrient calculations may be used to estimate calorie and protein needs in this population.
While these numbers may change based on disease factors, they may be a good place to start for the otherwise healthy, geriatric adult. A dietitian can assist in calculating nutrition needs.
- Energy/Calories: 25-35 kcals/kg of body weight
- Protein: 1.0-1.2 g/kg of body weight
- Fluids: 25-30 ml/kg
Calorie needs in this population may need to be on the higher end (35 kcals/kg) in order to maintain or gain weight if the patient has lost a concerning amount, or is at a BMI < 23.0 kg/m^2.4
Protein needs for older adults are generally be higher to maintain lean body mass and prevent muscle wasting. Lean meats such as chicken, yogurt, low-fat milk, eggs, and beans can increase protein in the diet.
The older adult population tends to be at a higher risk of dehydration. This may be due to a decrease in total body water. Or simply not feeling thirsty. Or even due to medication side effects. Dehydration can lead to a higher risk of falls and further impairment of ADLs.
Encouraging older adults to drink adequate fluids is important. A good rule of thumb is 1 ml of water for every calorie consumed. Of course, unless otherwise directed by the patient’s physician.
Each cup of water is about 250 ml of fluid. Therefore, if a person is eating 1800 calories, drinking about 7-8 cups of water a day should be enough.
It’s also important to remember that we get fluid in other ways – from fruits and vegetables, tea, juice, and other beverages, not just water.
Vitamin and Mineral Needs
A study published in the Journal of Nutritional Sciences published in 2017 stated that certain vitamins and minerals may be of concern. These include: vitamin B12, vitamin D, iron, calcium, and magnesium.5 Reasons for this may be due to lack of consumption. But may also be related to decreased absorption.
In aging adults, there is a decrease in acid secretion in the stomach – which is needed for the absorption of vitamin B12, calcium and iron.
Vitamins and minerals should come from food first. But not everyone can get their nutrition needs met by food. For these individuals, supplements may be necessary.
The National Institute of Aging states that individuals over the age of 50 should be mindful to get adequate calcium, vitamin D, vitamin B6, and vitamin B12.6
Their recommendations are:
- Vitamin B12: 2.4 micrograms/day.
- Calcium: 1,200 milligrams/day for women and 1,000 milligrams/day for men. (Individuals should not supplement more than 2,000 milligrams/day)
- Vitamin D: 600 IU (international units) for those aged 51-70 years old, and 800 IU for those over 70 years old (not to exceed 4,000 IU/day)
- Vitamin B6: 1.5 milligrams/day for women, and 1.7 milligrams/day for men.

Supplements are not monitored by the FDA.
Therefore, brands for supplements should be addressed by a primary care provider or dietitian as needed.
Individuals who believe they need supplements should always speak with their healthcare provider. Preferably, before supplements are started.
Some supplements (even vitamins and minerals) can cause drug interactions with medications you are already taking.
Beyond Nutrients: Nutrition at a Deeper Level
Beyond estimating nutrient needs, how does a dietitian play a role in geriatric failure to thrive?
Encourage Eating
Some older individuals may lack motivation to eat, or simply not have the appetite. Telling them they need to eat won’t do much. So how can we all help older individuals want to eat? Try these tips:
- Making food pleasurable: Many older adults simply cannot taste their food anymore. Making it tastier can encourage patients to eat more simply because it’s better. Adding herbs, spices, and fats can help increase flavor (plus, butter adds more calories!).
- Making meal time easier: Making sure they have access to food and that food is easy to prepare.
- Making meal times more social: We eat more together. Brainstorm ideas for who they can eat meals with. Perhaps they can visit a congregate meal site at a senior center. Or even have a visitor come to the home. It’s important to have company while eating to encourage a higher intake.
Increasing Caloric Intake
Other things that may help elderly patients increase calories include7:
- Frequent Meals & Snacks: Three small meals with high calorie snacks when the patient is hungry.
- High Calorie Drinks: Adding high calorie drinks and/or shelf stable nutrition drinks (Boost Plus, Ensure, etc.).
- Adding Fats: Adding oil, butter, cheese, cream, dressings, and sauces to meals and snacks to increase caloric intake.
- Adding Protein: Adding higher protein foods. This includes lean meats, cheeses, legumes, tofu, fish, milk, yogurt, etc. to every meal.
- Avoiding Diet Food: Avoiding foods labeled ‘diet’ or ‘low-fat’ or ‘low calorie’.
You can learn more in our High Calorie archive. And be sure to check out our High Calorie SHAKES e-Cookbook with delicious high calorie recipes.
Encouraging Physical Activity
Another thing that may help increase appetite and food consumption is exercise! Physical inactivity can contribute to functional decline in elderly adults. Making sure that the patient is physically active, if they’re able to be, is important. Exercise and movement can help stimulate appetite and help patients be more interested in food.
Working with a physical therapist or qualified personal trainer may be beneficial.
The Ds of Failure to Thrive
Before wrapping up, we wanted to share some additional information which may be helpful in understanding adult failure to thrive.
An article published in 2015 states that there are ‘11 D’s of Failure to Thrive’ which is a list of 11 things that may lead to geriatric failure to thrive.8
The 11 D’s of Failure to Thrive include:
- Diseases
- Dementia
- Delirium
- Drinking Alcohol
- Drugs
- Dysphagia
- Deafness, Blindness, or other Sensory Deficits
- Depression
- Desertion by friends or family
- Destitution
- Despair
Diseases
This may include medical conditions that are either undiagnosed or previously diagnosed. These can vary in duration and type. Chronic concurrent diseases may also be present. Diseases such as cancer and renal failure have been linked to a higher rate of failure to thrive.
Dementia
Dementia, or the loss of memory can also lead to failure to thrive due to forgetting family or friends, forgetting to eat or get groceries, etc.
Delirium
Characterized by cognitive impairment, delirium is a more acute loss than dementia, and can still cause failure to thrive.
Drinking alcohol, or using other substances
Those who drink more heavily than others tend to forget meals. Some people may prioritize alcohol over food. Older adults tend to process alcohol more slowly, leading to increased feelings of being drunk and higher risk of failure to thrive.
Drugs
Prescription medications, or non-prescription substances may be processed more slowly in older adults. This can lead to more fatigue and less ability to function to perform ADLs or IADLs. These factors can lead to failure to thrive.
Dysphagia (difficulty swallowing)
Dysphagia is common in older adults, especially those with stroke or certain cancers. Those who have a difficult time swallowing may opt to restrict food and drink because it is painful. They may also be afraid they will choke. This restriction may lead to weight loss and failure to thrive.
Deafness, blindness or other sensory deficits
As discussed before, loss of taste, smell, sight, or hearing can impact how individuals experience food, mealtime, and day-to-day life. These sensory impairments have the potential to lead to failure to thrive.
Depression
Depression can lead to less desire to eat or forgetting to eat. This can lead to adverse outcomes including weight loss and failure to thrive.
Desertion by family or friends
Social desertion or lack of communication or time spent with friends or family may lead to less desire to eat, feelings of loneliness, and feelings of depression that can lead to failure to thrive.
Destitution (socioeconomically disadvantaged)
Older individuals who live alone may not be able to afford groceries or meals purchased from restaurants, and may prioritize paying rent or for clothing rather than spending money on enough food for themselves.
Despair (wanting to give up)
Closely linked to depression, suicide and despair are not uncommon in older adults who may also be socially or economically disadvantaged or lonely. Despair can also cause individuals to eat less, potentially leading to malnutrition and failure to thrive.
Failure to Thrive is Not a Normal Part of Aging
It is important to recognize that failure to thrive is not an inherent or normal part of aging. Failure to thrive occurs when the above risk factors, or the D’s, are prevalent in someone’s life.
It is also important to recognize that an individual may or may not have multiple or all of the risk factors associated with failure to thrive. One individual may have failure to thrive and have five of the above risk factors, while another is suffering while just having one of the risk factors.
It is very important that if failure to thrive is suspected, the patient undergo a full examination and evaluation of risk factors, signs and symptoms, and severity.
This evaluation should be done by a physician. All other pertinent healthcare providers such as the registered dietitian or social worker should help when asked to, to provide the best plan of care.
Failure to Thrive Elderly Conclusion
Failure to thrive is relevant to anyone over the age of 65. It is also important for anyone working in a healthcare environment, and anyone who has family or friends who are reaching an older age.
Failure to thrive is a serious issue. FTT affects between 25-40% of residents in nursing homes. It also effects 5-35% of the elderly population living in a community setting or by themselves.9
Failure to thrive is a complex and difficult medical condition. It requires multiple healthcare providers. This may include a physician, a dietitian, a social worker, and possibly physical, occupational, and speech therapists if indicated.
Overall, treating and preventing further problems with nutrition is crucial. A dietitian can help to increase calories and encourage oral intake.
Sometimes the patient does not improve with various nutritional changes, or help from the healthcare team. Hospital care or assisted care may be needed to remedy the failure to thrive and to make sure the patient is improving in nutrition status.
Awareness of this condition, and knowing what can and should be done to prevent an increase in mortality or morbidity is important.
Let’s all work together to keep our loved ones and patients living their best life!
References
- https://www.aafp.org/afp/2004/0715/p343.html
- https://www.cancer.gov/publications/dictionaries/cancer-terms/def/adl
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3396084/
- https://thegeriatricdietitian.com/bmi-in-the-elderly/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5465850/
- https://www.nia.nih.gov/health/dietary-supplements
- https://bpac.org.nz/BPJ/2011/May/elderly.aspx#:~:text=The%20incidence%20and%20impact%20of,and%20protein%20meals%20and%20snacks
- https://emedicine.medscape.com/article/2096163-overview#a4
- https://www.freedomcareny.com/posts/failure-to-thrive-elderly#:~:text=Geriatric%20Failure%20to%20Thrive%20(FTT,are%20living%20in%20nursing%20homes
