Chronic Malnutrition in Seniors
Chronic Malnutrition in Seniors was written by Nicole Pabalan, freelance writer and dietetic intern at Oregon Health Sciences University. Reviewed/edited by Katie Dodd, MS, RDN, CSG, LD, FAND
What is Chronic Malnutrition?
Malnutrition is a serious condition among older adults.
Definition of Chronic Malnutrition
According to the World Health Organization (WHO), chronic malnutrition refers to prolonged deficiencies, excess, or imbalances in an individual’s daily dietary intake.
Malnutrition is often divided into several subcategories:
- Undernutrition refers to an inadequate intake of energy and nutrients, thus an individual’s dietary intake does not meet their nutritional needs. This nutritional disorder can result in undernourishment, poor absorption or the ability to properly use essential nutrients (Hunger and Malnutrition 2019).
- Micronutrition-related malnutrition refers to deficiency in vitamins and minerals.
- Protein-Energy Malnutritoin refers to inadequate intake of protein and calories leading to a loss of muscle and/or subcutaneous fat.
Studies indicate that malnutrition in the older adult’s demographic has become exponential. Compared to any other age group, older adults with chronic malnutrition are at greater risk for nutrition-related chronic diseases (Eggersdorfer et al., 2018). For example, deficiencies or excess dietary intake can contribute to heart disease, diabetes, and infections (e.g. pneumonia and influenza).
Contributing Factors
Some contributing factors related to chronic malnutrition include involuntary weight loss, consistent fluctuation in weight, and inability to consume the foods they need to maintain health.
Often, when individuals hear about “malnutrition,” our initial thoughts may depict someone who is frail and ill, however, that’s not always the case. Chronic malnutrition in older adults can exist regardless of body size.
According to the Academy of Nutrition and Dietetics, long-term dietary intake of excessive energy, poor-nutrient diet, and decrease in physical activity can cause overweight or obesity in individuals (2012). Seniors with excess body weight can still have have reduced muscle mass, functional limitations, and multiple nutrient deficiencies (Bernstein and Munoz, 2012).
Nutritional challenges are significant contributors to chronic malnutrition in older adults, however other reasons may include systemic healthcare, environmental, and biological factors (Eggersdorfer et al., 2018).
Research reveals that malnutrition-associated diseases in seniors within the United States has become an economic burden of approximately $51.3 billion. Healthcare costs for older adults with a form of chronic malnutrition increased the expense of healthcare due to the need for longer hospital stays, increased risks for falls, and other complications.
The Alliance for Aging Research provides a thorough explanation of malnutrition in the elderly:
Statistics in Older Adults
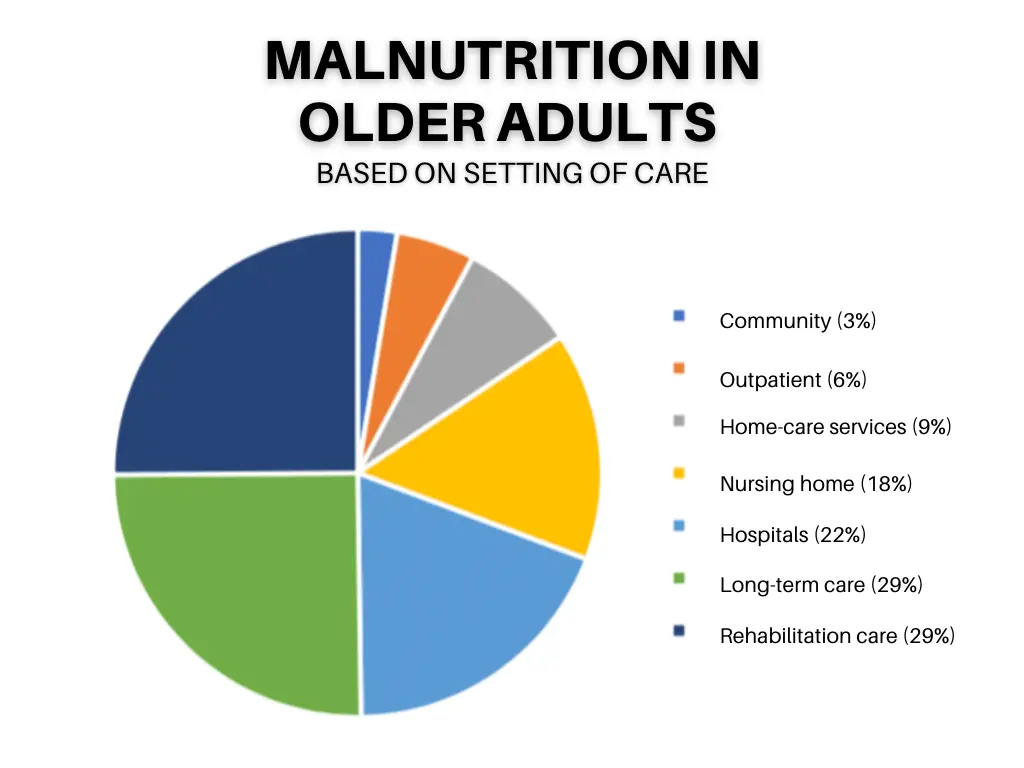
Figure 1: Prevalence of malnutrition in older adults based on different populations, healthcare settings, and the Mini Nutritional Assessment (Volkert et al., 2019)
In the U.S., the older adult demographic is rapidly increasing with the prediction of approximately 72.1 million seniors or almost 20% of the entire population. Thus, it’s imperative for elderly adults to obtain access to food and nutrition services, and supportive care to lead a healthy life with longevity.
The ultimate goal is to prevent the burden of ill health and to strive for the progression of aging to occur with minimal effects of disease and disability.
Signs/Symptoms of Chronic Malnutrition
The National Council on Aging (NCOA) describes signs and symptoms of Chronic Malnutrition in Seniors may include:
- Muscle weakness
- Fatigue
- Illness or infection
- Irritability or depression
- Involuntary weight loss
- Poor appetite,
- Easy bruising
- Dental problems
Causes of Chronic Malnutrition in Older Adults
According to the NCOA, the causes of malnutrition in seniors can occur for many reasons.
Some common contributing factors may include the following (Corcoran et al., 2019):
- Food insecurity (inability to get the food they need, often because of limited finances)
- Disordered eating (trouble chewing, swallowing, and impaired dental health)
- Loss of appetite
- Living alone or feeling of loneliness
- Side effects of prescribed medications
- Restricted diets
- Lack of mobility related to functional decline
- Psychological factors (i.e. depression and dementia)
- Impaired function of the gastrointestinal (GI) tract or GI disorders.
- Decreased senses of taste and smell increases risk of malnutrition almost three times more. Furthermore, older adults with impaired swallowing functions are five times more likely to become malnourished.
Deficiency and Malnutrition in Geriatrics
Older adults are at risk of deficiencies in vitamins and minerals because of poor-quality diets, and medical conditions or age-related factors that may impair the body’s ability to absorb nutrients (Doley, 2017).
Chronic malnutrition may lead to inadequate levels of vitamin D, which contributes to decline in bone density, reduced mobility, and a higher risk of falling. Deficiency related to chronic malnutrition in both vitamin D and calcium increase can induce the development of osteoporosis.
In addition, the ageing process includes decreased skin production or thinning of the skin, and decreased exposure to sunlight (vitamin D is produced in the skin when it’s exposed to the sun), which makes malnourished older adults even more at risk for osteoporosis (Corcoran et al., 2019).
Risks of Chronic Malnutrition
Seniors may experience age-related changes that impact the GI tract function. Thus, chronic malnutrition in older adults may cause further problems to organs in the digestive system and exacerbate other physiological and psychological health factors. Below is a list of organs and other factors that are associated with the effects of chronic malnutrition in older adults.
| How the body is affected by chronic malnutrition | |
| Digestive System | |
| Esophagus | may reduce mucous production, which can lead to dysphagia or impact of the movement of food passing through into the stomach (Carrera et al., 2012; Tagliaferri et al., 2019). |
| Pancreas | disrupts the body’s ability to convert the food we eat into energy that nourishes body’s cell to assist with digestion and other important functions |
| Small Intestine | prevents blood flow to our small intestines, which most of our digestion occurs |
| Large Intestine (Colon) | loses its ability to reabsorb water and electrolytes, which may cause diarrhea and increase risks of death in severely malnourished patients (Saunders & Smith, 2010)
|
| Other | |
| Immune System | delays wound healing and increases risks for infection (i.e. sepsis) |
| Psychological effects | May cause feeling of detachment, depression, anxiety, and self-neglect (Saunders & Smith, 2010) |
Food Insecurity
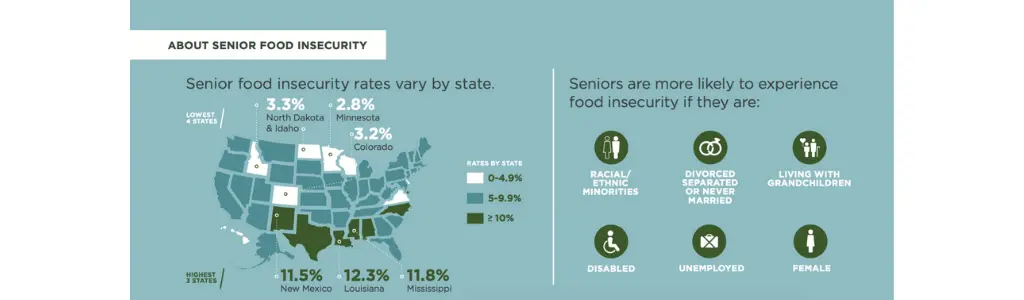
Food insecurity in older adults may increase risks of chronic malnutrition. Below is an infographic that displays the rates of elderly adults across the U.S. who are affected by food insecurity provided by Feeding America:
Some tools used to assess nutrition status for chronic malnutrition in older adults are listed below:
- Anthropometric measures such as usual body weight, body measurements, and hand grip strength.
- The Mini Nutrition Assessment (MNA) considers food intake, weight loss, mobility, BMI, psychosocial stress, dementia, and depression.
- Other tools used to assess nutrition status are associated with technology which includes the following:
- Dual Energy X-ray Absorptiometry (DXA): measures bone mineral density
- Computerized Tomography Scan (CT or CAT scan): is a rotating x-ray machine that provides details of soft tissues, blood vessels, and bones.
- Bioelectrical Impedance Analysis (BIA) estimates body composition with the consideration of body fat and muscle mass
Resources to access food for older adults at risk of chronic malnutrition
There are many resources available to help seniors get the food they need. Be sure to check out our article on Food Access for older adults. Additional resources are listed below.
The NCOA provides the following resources for seniors:
- Senior Supplemental Nutrition Assistance Program (SNAP) Initiative
- Designed to assist older adults to apply and enroll for SNAP benefits
- ncoa.org
- BenefitsCheck
-
- Free online service that can screen limited income seniors for benefits. This can connect eligible older adults to benefits programs across all 50 states.
- BenefitsCheckUp.org
-
Ways to Prevent Chronic Malnutrition in Older Adults
There are many things that can be done to prevent chronic malnutrition in older adults.
Fortified foods
Fortified foods are those that add extra calories to foods normally eaten. For example, adding dry milk powder to liquid milk boosts the calorie content. The list below provides examples of calorie boosting add-ins that can be used to fortify foods an older adult is already eating:
- Dry milk powder
- Protein powder
- Butter or margarine
- Olive oil
- Peanut Butter
- Honey or Agave
Consume smaller meals
This may seem counter intuitive…. getting someone to eat more by eating less. But sometimes just providing a bunch of food with a meal isn’t good enough. If they get full too fast, they can’t finish that big meal. Rather, provide smaller, frequent meals per day with high energy to help older adults with loss of appetite, achieve energy needs, and avoid prolonged fasting (American Society for Nutrition 2015).
Supplements
Depending on the type of malnutrition, some older adults may need supplements in addition to food.
Oral nutritional supplements that come in ready-made sip feeds or powders that can be mixed with milk or water are available (Strategies to Improve Nutrition in Elderly People). These drinks can be consumed in between meals. Check out our article on High Calorie Drinks to get some other good ideas for adding extra calories in between meals.
Food modifications
If an older adult is having swallowing or chewing problems, it can be hard to eat. This can contribute to malnutrition. Consider modification to food texture to ease the eating process (i.e. pureed, blended, or soft foods).

Interventions for Chronic Malnutrition in Seniors
Interventions for older adults with chronic malnutrition should be comprehensive and individualized to improve health status. It’s essential to take an interdisciplinary team approach that takes into account factors such as physical and mental/psychological, social, clinical, and ethical. Below is a list of healthcare professionals who may take part in a multidisciplinary approach for treating chronic malnutrition.
An interdisciplinary team for seniors with chronic malnutrition may include healthcare professionals such as:
-
- Speech-Language Pathologist
- Responsible for determining chewing or swallowing problems
- Pharmacists
- Evaluate prescribed medications and nutrient interactions
- Registered Dietitian
- Complete nutrition assessment, diagnosis, and develop evidence-based evidence
- Physician/ Nurse Practitioner
- To oversee overall care plan and make appropriate referrals to help address contributing factors of chronic malnutrition in older adults
- Social Workers/ Therapists
- To help older adults who may be experiencing depression or self-isolation in which contribute to symptoms (i.e. loss of appetite) that can increase risks or cause chronic malnutrition
- Physical Therapists
- Can help older adults regain strength and prevent further muscle loss
- Occupational Therapists
- Can help older adults who have difficulty eating and can benefit from adaptive eating equipment
- Speech-Language Pathologist
Additional Resources for Chronic Malnutrition in Older Adults
- National Institute on Aging – NIH
- American Society for Parenteral and Enteral Nutrition (ASPEN)
- Defeat Malnutrition Today
- Tips for Older Dietary Supplement Users
- Senior Food Insecurity – Feeding America
- Senior Nutrition Guide: Supporting Access to Healthy Food for Older Adults
Also be sure to check out our High Calorie Foods SERIES on RD2RD which includes a high calorie food list, grocery list, and meal planner to help prevent and treat malnutrition. There is also a High Protein Foods SERIES available.
Conclusion
There are several factors that contribute to chronic malnutrition within the geriatric population such as chewing and swallowing problems, disabilities, restricted mobility, cognitive impairment, depression, social isolation, food security status, acute disease, adverse side effects of medication, and restricted diets.
Chronic malnutrition in older adults may appear in those who experience involuntary weight loss and individuals who are overweight or obese. Dietary restrictions are not recommended for older adults experiencing unintended weight loss.
The good news is, chronic malnutrition in older adults CAN be prevented and reversed with early detection. Thus, it’s important for seniors to routinely screened for chronic malnutrition. Before considering to take any dietary supplements be sure to consult your physician.
References
- 5 Malnutrition Facts You Probably Didn’t Know. (2016, August 30). Retrieved September 03, 2020, from https://www.ncoa.org/healthy-aging/chronic-disease/nutrition-chronic-conditions/why-malnutrition-matters/5-malnutrition-facts-older-adults/
- 11, N., & Contributor, *. (2019, June 18). Small, Frequent Meals. Retrieved September 03, 2020, from https://nutrition.org/small-frequent-meals/
- Anderson, J. R., Berry, E., & Ferranti, P. (2019). Hunger and Malnutrition. In Encyclopedia of food security and sustainability (Vol. 2, pp. 315-335). Amsterdam: Elsevier.
- Carrera, Victor Gonzalez et al. “Acute esophageal necrosis in a patient with multiple comorbidity.” Annals of gastroenterology vol. 25,2 (2012): 162.
- Corcoran, C., Murphy, C., Culligan, E. P., Walton, J., & Sleator, R. D. (2019). Malnutrition in the elderly. Science Progress, 102(2), 171-180.
- Eggersdorfer, M., Akobundu, U., Bailey, R. L., Shlisky, J., Beaudreault, A. R., Bergeron, G., Blancato, R. B., Blumberg, J. B., Bourassa, M. W., Gomes, F., Jensen, G., Johnson, M. A., Mackay, D., Marshall, K., Meydani, S. N., & Tucker, K. L. (2018). Hidden Hunger: Solutions for America’s Aging Populations. Nutrients, 10(9), 1210. https://doi.org/10.3390/nu10091210
- Fact sheets – Malnutrition. (2020, April 1). Retrieved September 02, 2020, from https://www.who.int/news-room/fact-sheets/detail/malnutrition
- Fortification. (2017, April 12). Retrieved September 03, 2020, from https://www.nutritionintl.org/what-we-do/by-programs/fortification/
- Molfino, A., Gioia, G., Rossi Fanelli, F., & Muscaritoli, M. (2014). The role for dietary omega-3 fatty acids supplementation in older adults. Nutrients, 6(10), 4058–4073. https://doi.org/10.3390/nu6104058
- Rémond, D., Shahar, D. R., Gille, D., Pinto, P., Kachal, J., Peyron, M. A., Dos Santos, C. N., Walther, B.,
- Bordoni, A., Dupont, D., Tomás-Cobos, L., & Vergères, G. (2015). Understanding the gastrointestinal tract of the elderly to develop dietary solutions that prevent malnutrition. Oncotarget, 6(16), 13858–13898. https://doi.org/10.18632/oncotarget.4030
References Continued
- Saunders, J., & Smith, T. (2010). Malnutrition: causes and consequences. Clinical medicine (London, England), 10(6), 624–627. https://doi.org/10.7861/clinmedicine.10-6-624
- Strategies to improve nutrition in elderly people. (n.d.). Retrieved September 03, 2020, from https://bpac.org.nz/BPJ/2011/May/elderly.aspx
- Tagliaferri, S., Lauretani, F., Pelá, G., Meschi, T., & Maggio, M. (2019). The risk of dysphagia is associated with malnutrition and poor functional outcomes in a large population of outpatient older individuals. Clinical Nutrition, 38(6), 2684-2689. doi:10.1016/j.clnu.2018.11.022
- Tappenden, K. A., Quatrara, B., Parkhurst, M. L., Malone, A. M., Fanjiang, G., & Ziegler, T. R. (2013). Critical Role of Nutrition in Improving Quality of Care: An Interdisciplinary Call to Action to Address Adult Hospital Malnutrition. Journal of the Academy of Nutrition and Dietetics, 113(9), 1219-1237. doi:10.1016/j.jand.2013.05.015
- Volkert, D., Beck, A. M., Cederholm, T., Cereda, E., Cruz-Jentoft, A., Goisser, S., de Groot, L., Großhauser,
- F., Kiesswetter, E., Norman, K., Pourhassan, M., Reinders, I., Roberts, H. C., Rolland, Y., Schneider, S. M., Sieber, C. C., Thiem, U., Visser, M., Wijnhoven, H., & Wirth, R. (2019). Management of Malnutrition in Older Patients-Current Approaches, Evidence and Open Questions. Journal of clinical medicine, 8(7), 974. https://doi.org/10.3390/jcm8070974
