“Nutrition and Healing Wounds” was written by dietetic intern Rachel Evans and edited by Katie Dodd, MS, RDN, CSG, LD, FAND
Older adults have delicate skin which can be more susceptible to injury. Bruises and cuts happen to everyone, but the risk of these not healing properly and turning into more serious chronic wounds is increased as we age.
This article will cover the different types of wounds, preventative measures, barriers to healing wounds, ways to accelerate healing. And of course, the importance of good nutrition and healing wounds!
Types of Wounds
An “acute” wound is a wound that is temporary and heals without any complications. When a wound does not heal, stays the same or becomes worse, this is referred to as a “chronic” wound. Chronic wounds affect about 3 to 6 million people in the United States and 85% of the people affected are 65 years or older (1).
Multiple types of wounds are at risk of evolving into chronic wounds including diabetic ulcers, surgical wounds, venous ulcers, arterial ulcers and pressure injuries.
Diabetic Ulcers
Diabetic ulcers are a complication of diabetes. If a person with diabetes is unable to manage their blood sugars, it can lead to many different long-term complications including those that impact the healing of the skin.
How does this occur? There are several reasons. Chronic high blood sugar levels can lead to white blood cells not functioning as they should which increases the chance of infection (1, 2).
It can also weaken the arteries and narrow the blood vessels. This results in decreased blood flow which inhibits nutrients and oxygen from reaching the wound site.
Nerve damage can occur, causing a loss of sensation to that area. As a result, pain or discomfort from a wound may not be felt and early intervention may not be performed.
And finally, if the blood sugars continue to be elevated and an ulcer is not managed properly, infection, gangrene or even the need for an amputation may arise (1).
Surgical Wounds
Surgical wounds are incisions or wounds resulting from a surgical procedure. The size and location vary depending on what surgery was performed.
If sterile techniques are not used during the procedure and/or post operation hygiene is poor, the risk of infection at the wound site increases. Keeping the incision clean while it heals can prevent it from becoming a chronic wound.
Venous Ulcers
Venous ulcers form on the lower extremities of the body (legs, ankles and feet) and are often caused by impairment of the valves inside the veins.
When the valves are not working properly blood pressure in that area may be chronically high and blood does not circulate properly; this may result in the development of a venous ulcer.
Other issues with veins in the legs may cause blood to collect and swelling to occur. This built-up pressure poses a risk for the development of venous ulcers as well (3).
Arterial Ulcers
Arterial ulcers are also located on the lower extremities, and like venous ulcers they are a consequence of poor blood circulation. However, in an arterial ulcer the cause of poor blood flow is blocked arteries in the legs (4).
Pressure Injuries
Pressure Injuries, also known as bed sores and decubitus ulcers, are the most common type of chronic wound amongst older people (5). According to the Agency for Healthcare Quality and Research, pressure injuries affect up to 2.5 million people per year (6).
Studies show that two thirds of pressure injuries occur in people over 70 years of age and that people with severe pressure injuries have much higher mortality rates (6).
Although pressure injuries are completely preventable, 60,000 people die each year as a result of them (6). For this reason, we will primarily focus on pressure injuries and how nutrition in addition to proper wound care can help to heal them!

What Are Pressure Injuries?
Pressure injuries occur when there is ongoing pressure, friction, shearing and/or excessive moisture to an area of skin.
They can occur anywhere; however, most people (especially bed or wheelchair bound) form pressure injuries in more “bony” areas such as their tailbone or buttocks, spine, shoulder blades, hips, backs of arms, legs and heels (7).
Stages of Pressure Injuries
Wound care specialists categorize pressure injuries based on the stage of the wound. As the severity of the wounds increase, the potential complications along with the nutrition required to help heal the wound also increases.
Stage 1 Pressure Injury: Non-blanchable erythema of intact skin
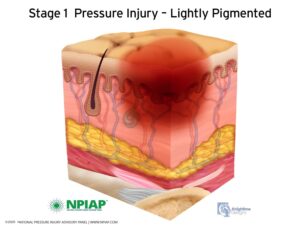
A stage 1 pressure injury may present as a discolored or bruised area of the skin. The area may feel warmer or cooler to the touch and may be irritated causing a burning or itching feeling (8,9).
Stage 2 Pressure Injury: Partial-thickness skin loss with exposed dermis

When a pressure injury becomes a stage 2, the bruised or discolored area begins to form an open wound. It may have a shallow bowl-like or open blister appearance. The dermis is exposed, although, fat and deeper tissues are not visible in this stage. The wound and the area surrounding it may be very painful (8,9).
Stage 3 Pressure Injury: Full-thickness skin loss

In a stage 3 pressure injury, the wound becomes deeper, exposing a layer of fat under the skin. Dead skin tissue called slough or eschar, may be visible (8,9).
Stage 4 Pressure Injury: Full-thickness skin and tissue loss

Stage 4 is the most severe stage of pressure injury. In this stage the wound continues to deepen, and a large amount of skin tissue is lost. Slough and eschar may be present and bone, muscle or tendons are visible in a stage 4 pressure injury (8,9).
Unstageable Pressure Injury: Obscured full-thickness skin and tissue loss

A wound is categorized as an unstageable pressure injury when large amounts of dead tissue is present, hiding the level of tissue damage below (8).
Deep Tissue Pressure Injury: Persistent non-blanchable deep red, maroon or purple discoloration

A deep tissue pressure injury may be an open or closed wound and it results from extreme or persistent pressure to the area. The skin is a deep red, maroon, or purple color. The wound may progress and show the actual degree of tissue injury, or may heal without tissue loss (8).
Complications
Many issues can come from having a pressure injury. One being a serious infection of the bone called osteomyelitis. Osteomyelitis occurs when infection in the skin tissue spreads to the bone. Another potential complication is sepsis. Sepsis is an infection of the blood and can be fatal (9).
Barriers to Healing Wounds
When the body is working to repair damage to the skin, there are several issues that may interfere and delay the healing process. It is important to minimize these barriers as much as possible.
Malnutrition

Nutrition status and wound healing are closely related. Malnutrition is when your body isn’t getting the nutrition it needs. Some indicators of malnutrition include unintended weight loss, not eating (or eating very small amounts), fat and muscle wasting, poor appetite, and weakness or fatigue.
A malnourished person is likely to experience delayed wound healing and an increased risk of infection (10). Therefore, it is extremely important to get proper nutrition for a person who is experiencing any of these signs. Not only to reach a healthy weight but to promote healing and immune function.
Immobility
Pressure injuries can develop in a matter of a few hours if movement does not occur (9). For this reason, bed and wheelchair bound people are at a high risk for pressure injuries.
For example, up to 85% of people who are paraplegic or quadriplegic develop a pressure injury just in the first month following their spinal cord injury as a direct result of immobility (5).
Many seniors face being confined to a bed or wheelchair every day as well; therefore, caretakers must be available to help them move.
Infection
Having an open wound is a big risk factor for infection. Bacteria has easy access to insides when the skin is no longer acting as a protective barrier.
The following factors play a role in the risk of infection:
- Location and size: If the wound is in an area that may be harder to keep clean or if a wound covers a large part of your body, it is more likely to become infected.
- Hygiene: Failing to keep the dressing clean by changing it frequently boosts the risk of bacterial growth and further skin breakdown.
- Immune function: Just as immunocompromised people are more likely to catch a cold or flu; their wounds are more likely to develop an infection. Their body also has a harder time fighting the infection off.
Healing Wounds and Stopping New Wounds
Now let’s talk about simple things you can do to help your body repair wounds and prevent new ones from forming.
Good Hygiene for Healing Wounds
Be very vigilant when it comes to hygiene. Change the wound dressing regularly to keep the area as clean as possible. If the dressing is becoming saturated with pus or blood, it needs to be changed more often (11).
If incontinence is an issue, changing clothing, disposable briefs, and bedding frequently is a must, especially if a wound in the buttocks or pubic region is present.
Once the wound is healed it is important to continue to have good hygiene by keeping skin clean and dry to prevent a new wound from forming.
Control Blood Sugars
For those with diabetes, keeping blood sugars within their normal range is needed for optimal healing and for preventing wounds.
If your medical provider or dietitian has instructed you to follow a diabetic diet or if you are currently prescribed medication to help with blood sugar control, you should follow the diet and take the medication as directed (2).
Frequent Position Changes
Any type of movement helps to relieve pressure, increase blood flow and decrease inflammation. If independent movement is not an option, frequent repositioning with a care takers help is necessary, even if that means just rolling from one side to the other.
It is recommended to change positions every 15 minutes or at least once per hour for people who are in a wheelchair and at least once every 2 hours for people who are lying in bed. Placing a pillow in between knees when lying on one side and elevating heels off the bed using a foam pad will also help in relieving pressure in these bony areas (9).
Specialty support surfaces, like alternate air mattresses can also be used to prevent further skin breakdown in a person who cannot get out of bed (11).
Nutrition and Healing Wounds
Now let’s talk about nutrition and the MAJOR role it plays in healing wounds! The human body works hard to heal a wound; therefore, people with wounds have higher energy and nutrient needs.
Balanced Diet and Hydration
The USDA recommends eating a minimum of 5-6 oz of protein, 2-3 servings of dairy, 2 cups of fruits, 6 servings of grain products, and 2.5 cups of vegetables daily (12). These recommendations are meant for generally healthy people.
For wound healing, eating more than what’s recommended here may be necessary, but sticking with including foods from each food group is key. By eating a wide array of foods, you are supplying your body with all the vitamins and minerals it needs for wound healing.
In addition to a well-balanced diet drink at least 8-10 cups of water each day, this will help with hydration and promote good blood flow (9).
Meeting Calorie Needs
When your body is working hard to heal wounds, it is burning more calories. This means you will need to eat more calories. Eating 3 meals and 2-3 snacks daily to meet nutrition needs for healing is important. Most adults will need 30-35 calories per kg of body weight to heal a wound (2).
If a poor appetite is making it difficult to eat large volumes, be sure to eat foods that are high in calories and protein. Getting the most nutrition from a small volume.
Some examples of these foods high calorie foods are nuts, cheese, whole milk, full fat yogurt or whole milk cottage cheese.
Protein and Healing Wounds
Getting enough protein in your diet is necessary for maintaining muscle and to heal wounds. Most adults need 0.8 grams of protein per kg body weight. During wound healing those needs increase to 1.25 to 1.5 grams of protein per kg body weight (2).
It is important to work with your healthcare team and/or dietitian to determine the right amount of protein you need based on your current medical conditions.
Be sure to check out our High Protein Foods SERIES on RD2RD which includes a high protein food list, grocery list, and meal planner!
Food Sources of Protein
Good food sources of protein include:
- Meat
- Poultry
- Fish
- Tofu
- Beans
- Quinoa
- Eggs
- Nuts
- Nut butters
- Milk
- Cheese
A good rule of thumb is to aim to include 20-30 grams of protein at each meal and 10-15 grams of protein at each snack (13). Below are some examples of serving size and protein content of some protein rich foods:
- 3 oz of meat or fish= 20-25 grams
- 8 oz of milk = 8 grams
- 2 tablespoons of peanut butter = 7 grams
- 8 oz of yogurt = 5-8 grams
- 8 oz Greek yogurt = 15-20 grams
- ½ cup cooked beans = 8 grams
- 1 egg = 6 grams
- ½ cup of firm tofu = 10 grams
- 1 slice of cheddar cheese = 7 grams
- ½ cup cooked quinoa = 4 grams
High Protein Snack Ideas
Eat 2-3 snacks in between meals to ensure you are getting the calorie, protein, vitamins and minerals you need to heal.
Here are some protein-packed snack ideas:
- Hard Boiled Eggs
- Greek yogurt parfait with fruit, nuts and seeds
- Protein Smoothie:
- Fruit, Spinach or Kale, Greek yogurt, whey protein powder, chia seeds and milk blended
- Egg and Avocado Toast
- Meat and cheese plate
- Trail Mix~ nuts, seeds and dried fruit
- Chicken salad and crackers
- Black Bean dip with veggies
- Smoked salmon and cream cheese on crackers
- Chia Pudding
- Chia Pudding Recipe: 1/3 cup chia seeds, 1 1/2 cups milk, 2 TBSP pure maple syrup, 1/2 TSP vanilla- mix and chill in fridge overnight

Vitamins and Minerals
National Pressure Injury Advisory Panel (NPIAP) guidelines recommend a person with a pressure injury should only take vitamin and/or mineral supplements when there is a confirmed or potential nutrient deficiency (2).
Eating well-balanced meals and snacks will likely be sufficient in most cases; however, it is a good idea to take a daily multivitamin with minerals if diet is inconsistent.
For example, someone may eat well one day and very little the next or they may be limited in what they can eat due to poor dental health; in this case a multivitamin would be beneficial.
Talk with your medical provider or dietitian to find out what vitamins and minerals may be right for you.
The following vitamins and minerals offer benefits that may help accelerate healing so including nutrient dense foods in your diet is important.
Vitamin A
Vitamin A supports cell reproduction, immune function and reducing inflammation (2).
| Daily Recommended Intake (DRI): 900 mcg/day for males and 700 mcg/day for females |
| Good Sources of Vitamin A: Kale, Carrots, Spinach, sweet potatoes, squash |
B Vitamins
There are many variations of B Vitamins (B1, B2, B3… and so on). In general, the B vitamins help in processing foods to make energy for new cell to grow, they also play a role in linking collagen together and immune function (2).
| Daily Recommended Intake (DRI): Each variation of the B vitamins has a different DRI. Eating a well-balanced diet will provide you with the B vitamins you need. |
| Food Sources of B Vitamins: Meat, Fish, Dairy, fortified cereals, whole grains, some fruits and vegetables |
Vitamin C
Vitamin C is an antioxidant; it protects cells from being damaged by free radicals. Vitamin C helps with making collagen as well as absorbing iron. Iron supplies the wound with oxygen which needed for healing wounds (2).
| Daily Recommended Intake (DRI): 90mg for men and 75mg for women |
| Food sources of Vitamin C: Oranges, red and green peppers, kale, brussels sprouts, broccoli, strawberries, grapefruit, kiwi |
Vitamin D
Vitamin D supports cell growth, immune function and reduces inflammation. (11)
| Daily Recommended Intake: 600 IU a day (800 IU for males over 70 years of age) |
| Foods Sources of Vitamin D: fortified cereal, fortified milk, fish with high fat content such as salmon |
Vitamin E
Vitamin E in an antioxidant and has been associated with healing and fading scars on the skin.
| Daily Recommended Intake: 15mg/day |
| Food Sources of Vitamin E: Almonds, Spinach, sweet potato, avocado, sunflower seeds, butternut squash, fish, olive oil, dark leafy greens, some fruits such as kiwi, blackberries, mangos, peaches |
Zinc
Zinc is a trace mineral. It supports immune function and helps our body to produce collagen. Zinc deficiency has shown to cause delayed wound healing. It is important that you are not deficient in zinc.
| Daily Recommended Intake: 8 mg/day for females, 11 mg/d for males |
| Food Sources of Zinc: Oysters, Beef, Chicken, Tofu, Pork, Nuts, Lentils, Yogurt, Oatmeal, mushrooms |
Amino Acids
Other nutrients typically associated with increased wound healing include amino acids such as glutamine, arginine, hydroxymethyl butyrate (HMB- a metabolite of the amino acid leucine) (2).
Amino acids are the building blocks of protein. Getting adequate protein in your diet should ensure you are getting these nutrients. Research is ongoing as to the benefit of wound healing and supplementing glutamine, arginine, and HMB.
Oral Nutrition Supplements
*This section includes affiliate links. As an Amazon Associate, I earn from qualifying purchases.
Getting adequate nutrition for wound healing can be a challenge for some older adults. Shopping and preparing meals might not be an option and that can play a major role in the quality of their diet.
In addition, poor dental health can make chewing and swallowing difficult (a barrier for getting enough protein)
In these cases, incorporating an oral nutrition supplement to meet calorie and protein needs may be a good idea. Examples of these that can be found over the counter are Ensure*, Boost*, Boost Glucose Control*, and Glucerna*. Generic versions are fine too.
Abbott Nutrition also makes a nutrition supplement specific for wound healing called Juven*.
Keep in mind you can make your own high calorie shakes along with taking a multivitamin.
Role of the Dietitian
A registered dietitian can help you with the following:
- Calculate nutrition needs for healing and recovery specific to you
- Assess your diet to ensure you are getting the nutrients you need
- Recommend modifications for those with chewing difficulty
- Provide meal and snack ideas and recipes
- Recommend vitamin and mineral supplementation if needed
- Recommend oral nutrition supplements if needed
Nutrition and Healing Wounds Conclusion
In seniors, acute wounds can quickly progress into chronic wounds and chronic wounds pose a big risk for further complications, some even life threatening. Therefore, wounds of all types and sizes need immediate attention and treatment.
Minimizing barriers to healing such as immobility and infection while optimizing nutrition can make a major difference in the healing and prevention of a pressure injury. Healing wounds with good nutrition starts from the inside out.
References:
- Guo S, Dipietro LA. Factors affecting wound healing. Journal of dental research. 2010; 89(3):219-299.
- Friedrich L, Collins N. Nutrition & Wound Healing In The Older Adult: Considerations For Wound Clinics. Today’s Wound Clinic. 2013; 7(9).
- Venus Ulcers. John Hopkins Medicine website. https://www.hopkinsmedicine.org/health/conditions-and-diseases/venous-ulcers.
- Arterial Ulcer. Vascular Society website. https://www.vascularsociety.org.uk/patients/conditions/12/arterial_ulcer.
- Agrawal K, Chauhan N. Pressure ulcers: Back to the basics. Indian J Plast Surg. 2012;45(2):244–254.
- Pressure Ulcers: An Underappreciated Public Health Issue. GeriPal blog. https://www.geripal.org/2016/03/pressure-ulcers-underappreciated-public.html.
- Pressure Ulcer. Wound Care Centers website. https://www.woundcarecenters.org/article/wound-types/pressure-ulcer.
- NPUAP Pressure Injury Stages. NPUAP website. https://cdn.ymaws.com/npuap.site-ym.com/resource/resmgr/npuap_pressure_injury_stages.pdf.
- Pressure Injuries. John Hopkins Medicine website. https://www.hopkinsmedicine.org/health/conditions-and-diseases/pressure-injuries.
- Stechmiller J. Understanding the Role of Nutrition and Wound Healing. Nutrition in Clinical Practice. 2010; 25(1).
- Bedsores (pressure ulcers). Mayo Clinic website. https://www.mayoclinic.org/diseases-conditions/bed-sores/diagnosis-treatment/drc-20355899.
- 2015-2020 Dietary Guidelines for Americans. USDA website. https://www.choosemyplate.gov/node/5658.
- Grieger L. Five Nutrition Tips to Promote Wound Healing. Academy of Nutrition and Dietetics website. https://www.eatright.org/health/wellness/preventing-illness/nutrition-tips-to-promote-wound-healing.
