COVID-19 and Older Adults
COVID-19 and Older Adults was written by Jennifer Spindola, NDTR, CDM, CFPP & reviewed/edited by Katie Dodd, MS, RDN, CSG, LD, FAND.
DISCLAIMER: The science around COVID-19 is constantly changing. Please refer to the CDC website for the most current COVID-19 guidance and your medical provider for any medical concerns.
2020 has been quite the year. Coronavirus, also known as COVID-19, has taken the world by storm. While it has affected everyone, it has certainly taken a toll on older adults. Social isolation and fear over contracting COVID-19 are serious issues among the elderly population. This article reviews some of the science and what we know about COVID-19 and older adults.
SARS-CoV-2 – COVID-19
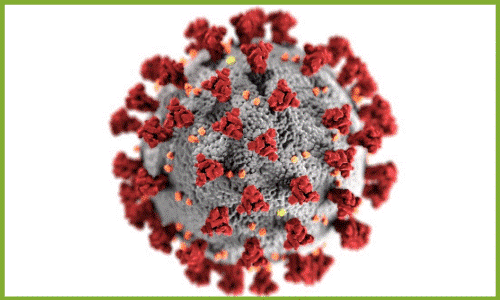 COVID-19 is the disease caused by SARS-CoV-2. This new positive-sense, single-stand, enveloped RNA virus – SARS-CoV-2 – has caused the first severe pandemic of the 21st century. According to researchers, it is more infectious and dangerous than influenza (1).
COVID-19 is the disease caused by SARS-CoV-2. This new positive-sense, single-stand, enveloped RNA virus – SARS-CoV-2 – has caused the first severe pandemic of the 21st century. According to researchers, it is more infectious and dangerous than influenza (1).
The Centers for Disease Control (CDC) reports 5,643,812 total cases and 175,651 total deaths from COVID-19 in the United States as of August 23, 2020 (2). Scientists from across the globe are unsure if this will be another endemic virus or if it will die out.
A second wave of COVID-19 is predicted for the fall of 2020 (3). If you wish to review the most recent COVID-19 U.S. case trends, click on the CDC link here.
COVID-19 Symptoms
 When exposed to the virus, it takes an average of 2-14 days for symptoms to appear.
When exposed to the virus, it takes an average of 2-14 days for symptoms to appear.
These symptoms may include nausea, vomiting, diarrhea, loss of taste/smell, shortness of breath (SOB), cough, fever, headache, body aches and sore throat.
Additionally, patients seen in the emergency room also report chest pressure, altered mental status, and/or appear to have bluish lips and face (4).
COVID-19 Testing
The primary test used to rule out COVID-19 is the Real-Time Reverse Transcriptase (RT-PCR) Diagnostic Panel. Earlier reports from China suggest the test provides ~30% false-negative results (5).
Currently, the CDC and the medical community believe that the RT-PCR test should not be the sole diagnosis test. Rather, clinical observations (e.g. nutrition-focused physical exam), chest X-Rays (e.g. observation of ground-glass opacities), and biomarkers (e.g. blood pressure and blood tests, including elevated Ferritin, LDH, D-Dimer, and CRP) should be considered for COVID-19 patient management decisions (6).
On July 2, 2020, the FDA provided emergency use authorization for a new test – SARS-CoV-2 (Flu SC2) Multiplex Assay – which will help medical professionals to detect (using one oropharyngeal or nasopharyngeal swab) – influenza viruses A and B as well as SARS-CoV-2. (7).
Off-Label COVID-19 Treatments
 At the end of August 2020, the USDA issued an emergency use authorization for convalescent plasma to treat Covid-19 in critically ill patients, which is wonderful news (14).
At the end of August 2020, the USDA issued an emergency use authorization for convalescent plasma to treat Covid-19 in critically ill patients, which is wonderful news (14).
However, at this present time, there are no FDA-approved medications for the treatment (or prevention) of COVID-19. Various antibiotics are used if the COVID-19 patient develops bacterial pneumonia or sepsis.
Currently, some off-label treatments for COVID-19 include:
- Antivirals (favipiravir and merimepodib)
- Malaria drugs (hydroxychloroquine and chloroquine)
- Anti-inflammatory (dexamethasone – corticosteroid) (13)
COVID-19 – Malnutrition
From a nutrition standpoint, there is a risk of malnutrition in many COVID-19 patients. They often experience a loss of appetite, especially those living with medical conditions such as COPD, diabetes, dementia, and cardiovascular disease.
As a whole, malnutrition can affect one’s immune system and disease susceptibility.
Recent Nutrition-Related Research and COVID-19
Recent studies found certain functional foods complement the treatment of COVID-19 at home. Think of good nutrition as a part of self-care. However, always follow your doctors advice when treating COVID-19 at home.
Keep in mind, if someone develops symptoms of chest pressure, altered mental status, and/or appear to have bluish lips and face, or any concerning symptoms DO NOT DELAY: Seek immediate emergency treatment.
Honey and COVID-19
The recent issue of Malaysian Journal of Medical Sciences noted in a letter to the editor that at least 50% of patients with COVID-19 will develop a secondary bacterial infection. And, that studies done on honey have shown antibacterial activity against gram (+) and (-) bacteria (8).
This means honey may be helpful in preventing that that secondary bacterial infection.
Hydration and COVID-19

Anyone with COVID-19 should be sure to drink plenty of water. Some prescribed medications can cause dehydration. This can negatively affect the kidneys.
And, COVID-19 patients are at higher risk of developing an acute kidney injury (AKI).
This spring, of the 1,000 admitted COVID-19 patients at New York-Presbyterian/Columbia University Irving Medical Center, 33.9% were also diagnosed with an AKI during the disease process (9).
Learn more about dehydration in the elderly by clicking here.
Zinc and COVID-19
Eat foods containing Zinc. This essential mineral is found in red meat, beans, nuts/seeds, eggs, and whole grains.
The International Journal of Infectious Diseases published a study of 4 patients with COVID-19 who were given high-dose oral Zinc salts in an outpatient setting. The patients were given different forms of Zinc (acetate, gluconate, citrate). And timing of therapy was not consistent (provided at different times of the disease course). However, all participants did see rapid resolution of shortness of breath (SOB), a hallmark symptom of COVID-19 (10).
Whether Zinc comes from food or a supplement therapy, it helps regulate innate and adaptive immune responses. Thus, possibly preventing a “cytokine storm” seen in COVID-19 patients (11).
Fermented Foods and COVID-19
Eat more fermented foods like kimchi and sauerkraut.
A study recently published in Clinical and Translational Allergy, found that patients in European countries who consumed more fermented foods had considerably lower deaths from COVID-19.
Researchers used the Johns Hopkins Coronavirus Research Center and analyzed European data on mortality rate per one million residents. They found that certain regions (e.g. Germany, Austria, Poland, Slovakia, and the Baltic region fared better than UK, Belgium, France, Italy, and Spain).
The researchers conclude fermented foods act as natural virus blockers. They do this by reducing the angiotensin-converting enzyme (ACE2). SARS-CoV-2 uses this receptor to get inside the cell to replicate (12).
Other Studies
Clinicaltrails.org lists 3,086 clinical studies related to COVID -19 as of August 23, 2020. While Zinc is mentioned in this blog for its possible treatment of COVID-19, there is little additional clinical evidence to support its efficacy in managing the disease.
There is still so much we don’t know, but one thing is for sure. Eating a healthy and balanced diet along with adequate hydration can help. Be on the lookout for more research to be published Vitamin C and D and COVID-19 patients.
Four Immune-Boosting Foods
For those readers concerned with COVID-19 this upcoming fall, consider consuming immune-boosting foods daily. While there is no evidence-based research available to support they help to prevent COVID-19, these foods can help control inflammation (the precursor to diseases). Again, eat a healthy and balanced diet. And drink plenty of water.
Citrus Fruits
Citrus Fruits like oranges and grapefruit contain a rich natural source of Vitamin C. Vitamin C may increase the production of white blood cells. Therefore, this can help protect the body against infection.
Garlic
The compound in raw garlic, allicin, have been associated with inhibition of viral infections. Meaning it could help keep your immune system strong.
Green Tea
Green tea contains catechins (class of flavonoids) which inhibit viral infections. It does this by blocking enzymes needed for DNA replication.
Walnuts
This super food is rich in Zinc, Vitamin B, Copper and Iron, all of which can boost one’s immunity. Walnuts also contain Vitamin E, a natural blood thinner, which can help reduce risks of clotting.
We also suggest that you also read our blog article, Seven Key Nutrients for Senior Nutrition, by clicking here.
COVID-19 and Older Adults Conclusion
We hope that you found this article about COVID-19 and older adults informative. This article just touched the surface on current research and good nutrition tips.
It is important that you stay connected with your primary care physician and specialists. These medical professionals are excellent sources of health information during this pandemic.
Stay safe and take care.
REFERENCES
1. Rettner, R. (2020, May 14). How does the new coronavirus compare with the flu? livescience.com. https
2. CDC COVID data tracker. (n.d.). CDC. https://www.cdc.gov/
3. Strazewski, L. (2020, May 8). Harvard epidemiologist: Beware COVID-19’s second wave this fall. American Medical Association. https://www.ama-
4. Coronavirus disease 2019 (COVID-19) – Symptoms. (2020, May 25). Centers for Disease Control and Prevention. https://www.cdc.
5. Lanese, N. (2020, April 3). Even if you test negative for COVID-19, assume you have it, experts say. livescience.com. https://www.
6. CDC 2019-Novel Coronavirus (2019-nCoV) Real-Time RT-PCR Diagnostic Panel. (2020, July 13). U.S. Food and Drug Administration. https://www.
7. CDC’s Diagnostic Multiplex Assay for Flu and COVID-19 and Supplies. (2020, July 3). Centers for Disease Control and Prevention. https://www.cdc.
8. Mustafa, M. Z., Shamsuddin, S. H., Sulaiman, S. A., & Abdullah, J. M. (2020). Anti-inflammatory properties of stingless bee honey may reduce the severity of pulmonary manifestations in COVID-19 infections. Malaysian Journal of Medical Sciences, 27(2), 165-169. https://doi.org/10.
9. Phend, C. (2020, May 29). Acute kidney injury seen in most severe COVID-19 cases. Medical News and Free Online CME | MedPage Today. https://www.
10. Finzi, E. (2020). Treatment of SARS-Cov-2 with high dose oral zinc salts: A report on four patients. International Journal of Infectious Diseases. https://doi.org/10.
11. Arshad, M. S., Khan, U., Sadiq, A., Khalid, W., Hussain, M., Yasmeen, A., Asghar, Z., & Rehana, H. (2020). Coronavirus disease (COVID‐19) and immunity booster green foods: A mini review. Food Science & Nutrition. https://doi.org/10.
12. Bousquet, J., Anto, J. M., Iaccarino, G., Czarlewski, W., Haahtela, T., Anto, A., Akdis, C. A., Blain, H., Canonica, G. W., Cardona, V., Cruz, A. A., Illario, M., Ivancevich, J. C., Jutel, M., Klimek, L., Kuna, P., Laune, D., Larenas-Linnemann, D., & Zuberbier, T. (2020). Is diet partly responsible for differences in COVID-19 death rates between and within countries? Clinical and Translational Allergy, 10(1). https://doi.
13. Marshall, W. (2020, July 3). COVID-19 (coronavirus) drugs: Are there any that work? Mayo Clinic. https://www.
14. Gupta, S., Gumbrecht, J., & Fox, M. (2020, August 24). US FDA announces emergency authorization for convalescent plasma to treat COVID-19. CNN. https://www.cnn.com/2020/
