BMI in the elderly is an important topic. There are a lot of misconceptions about BMI in the elderly that can cause harm, hospitalization, and early death in this population. As a Registered Dietitian, this is a topic near and dear to my heart.
In this article, I will be digging deep into BMI, appropriate BMI ranges in the elderly, and how to properly assess weight in the older adult.
Here is a sneak peak of the five main points of this article:
- BMI guidelines are different for older adults
- Overall health is more important than BMI
- Usual body weight is the best way to “assess” weight in the elderly
- Unintended weight loss must be stopped
- Older adults who want to lose weight should work with a dietitian
The BMI Backstory
Before we dig too deep, we need to look into what BMI is. How it is calculated. Where did it came from. And whether it is it here to stay. Then we’ll jump right into BMI in the elderly!
What is BMI?
BMI is the acronym for Body Mass Index. It is a tool commonly used to assess weight. Both height and weight are used to calculate BMI. This number is then classified as “underweight”, “normal”, “overweight”, or “obese” (1).
Standard BMI Ranges (1)
| Category | BMI |
| Underweight | <18.5 |
| Normal | 18.5 – 24.9 |
| Overweight | 25 – 29.9 |
| Obese | 30+ |
Often times in a health care setting, those with a BMI of 25 or greater (in the “overweight” or “obese” categories) are encouraged to lose weight. However, making such a recommendation for an older adult could be detrimental to their health. Research has shown us that BMI ranges are different for older adults.
How to Calculate BMI
BMI is calculatied using height and weight. You can always use an online calculator to do the math for you.
Here are two formulas that can be used for calculating BMI (depending on how you measure height and weight):
- English BMI Formula (using pounds and inches)
- BMI= (703 x Weight in lbs) / (Height in inches x Height in inches)
- Metric BMI Formula (using kilograms and meters)
- BMI= Weight in kg / (Height in meters x Height in meters)
The History of BMI
There is controversy over the use of BMI in health care. So, before we go further, let’s look at the history of BMI.
BMI, also known as Quetelet’s index, was developed in the early 1800’s by a Belgian mathematician. This data was published in a book looking at the distribution of height and weight among the “average man” (2).
It should be noted that Quetlet’s index was never intended to assess health status or mortality. BMI was simply an statistical index created by a mathematician nearly 200 years ago.
In the early 1900’s the index was incorporated into weight tables for life insurance companies. Then in 1980 the Clinical Director of the National Institute on Aging converted these height and weight tables used for life insurance into BMI. He determined that there was association between BMI and mortality (2).
This is the very condensed and simplified history of BMI. But, it is certainly interesting to take a look back to where BMI comes from.
BMI has its Limitations
Keep in mind that BMI is only one indicator of health. BMI assesses for weight and height, but it does not account for body composition (how much muscle or fat you have). A body builder may have a high BMI, but they are certainly not obese.
BMI also does not account for lifestyle factors like diet quality, physical activity, and overall health. You can be in the “normal” category and be very unhealthy. You can also be in the “obese” category and be very healthy.
We also know that health can exist at every size. And weight discrimination is a real issue. There are many health care professionals who advise against using BMI, for very valid reasons.
But the reality is that most health care institutions continue to use BMI. BMI is here to stay, so we need to make sure that older adults are assessed for BMI using the correct ranges.
BMI in the Elderly
When using BMI in the elderly, we need to make sure that the appropriate ranges are being used. To figure out the ideal BMI ranges for older adults, let’s look at some amazing research.
BMI and All-Cause Mortality in Older Adults
A wonderful meta-analysis came out in 2014 by Winters et al. looking at BMI and all-cause mortality in adults over age 65 (3). Basically, they looked at BMI ranges and the risk of death by any cause.
A meta-analysis is a big study that looks lots of little studies. Individual research studies are so important, but there are so many “what ifs” to consider. A meta-analysis looks at the big picture, examining a lot of different studies. So the results of a meta-analysis are super strong and reliable.
This particular meta-analysis looked at 32 different studies and included 197,940 older adults (ages 65+) with an average follow-up of 12 years (3). This is good, reliable data. No fake news here.
The Results
What researchers found was a u-shaped relationship between BMI and mortality. This means that rates of mortality were higher at the lower and upper end of the BMI spectrum. Here is an illustration of the findings:
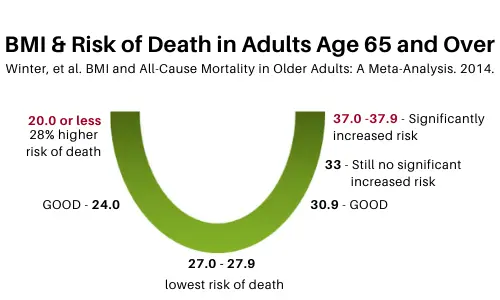
At the bottom of the “u”, the sweet-spot with the lowest rates of mortality, was when an older adult had a BMI of 27-27.9. Researchers found that older adults were still good up to a BMI of 30.9… interestingly even at a BMI of 33 they did not see a significant increase in mortality (3).
It wasn’t until BMI reached 37-37.9 that they saw a significant increase in mortality.
And even more interesting, on the flip side, rate of mortality increased much quicker with lower BMIs. Researchers found that a BMI down to 24 was still good, but when BMI reached 20 or below, rates of mortality increased by a whopping 28% (3).
So what was the conclusion of this study? Researchers concluded that for older populations, being overweight was not found to be associated with an increased risk of mortality. However, there was an increased risk for those at the lower end of the recommended BMI range for adults (3).
Because the risk of mortality increased in older people with a BMI <23.0, researchers recommended monitoring weight status in this group to address any modifiable causes of weight loss promptly (3).
Meaning… stop unintended weight loss, and quick!
A 2023 study looked into the impact of weight loss on mortality in older adults. Researchers found that in men a weight loss of >10% body weight increased mortality by 289%. And in women a weight loss of >10% body weight increased mortality by 114% (ref).
In a nutshell, low BMI and loss in weight contributes to increases in mortality in older adults.
BMI Chart for Older Adults
Since we typically see BMI in a chart format, I wanted to create a BMI chart for older adults. This is a table that I have created based on the research done by Winters et al. If you need to use BMI in the elderly, this chart is a good place to start for interpreting BMI results.
What Winters’ research tells us is that when it comes to BMI and all-cause mortality in older adults, the optimal BMI for those >65 years is likely between 23-30. BMI guidelines are higher for older adults.
BMI Ranges for Elderly
| Category | BMI |
| Underweight | <23 |
| Normal | 23 – 30 |
| Overweight | >31 |
BMI in Adults vs. BMI in Older Adults
Now let’s compare the BMI Charts for adults vs. older adults.
| Category | BMI Range for Adults | BMI Range for Older Adults |
| Underweight | <18.5 | <23 |
| Normal | 18.5 – 24.9 | 23-30 |
| Overweight | 25 – 29.9 | >31 |
| Obese | 30+ |
You can see that the “normal” for older adults (23-30, the ranges where we see the lowest rates of mortality) is in the “overweight” category in the standard BMI table for adults.

All too often older adults with a BMI between 25-29.9 are told to lose weight… for their health. But they are already in the best range of BMI for their age (with the lowest risk of mortality!).
And weight loss in older adults can lead to muscle loss. Older adults have less muscle to start with (we’ll dive into that soon).
So the reality is that promoting weight loss to “normal” based on the standard BMI ranges for adults (18.5-24.9) can increase the risk of mortality and poor health outcomes in older adults.
This is so important to know. And not enough people realize this. We need to spread the word and STOP encouraging weight loss in older adults who already have a BMI in the lowest rates of mortality.
OK, I’ll step off my soap box and we’ll dive deeper into why BMI ranges are higher in older adults.
Why Higher BMI in the Elderly?
Why is a higher BMI in the elderly associated with lower rates of mortality? There are many pieces to this puzzle. But the biggies come down to: sarcopenia, body composition, and frailty.
Our bodies change with age. This cannot be ignored.
Sarcopenia in Older Adults
Sarcopenia is defined as the decline of skeletal muscle tissue with age (muscle loss). It is a major cause of functional decline and loss of independence in older adults (4).
Sarcopenia actually starts when we are quite young, generally around age 30. And the loss of muscle mass continues each year. This illustration is an example of muscle mass at age 25 compared to age 75.

Loss of muscle is one of the main reasons unintended weight loss is so detrimental in older adults.
When unintended weight loss occurs, older adults are losing muscle which:
- increases their fall risk
- decreases their ability to do daily tasks (getting dressed, cooking, etc.)
- decreases their level of independence
- increases their risk of mortality
Research in Sarcopenia

A research article published in 2014 examined the impact of obesity on sarcopenia and mortality risk (5).
Researchers found that older women with sarcopenia had an increased all-cause mortality risk independent of obesity (meaning it didn’t matter whether they were obese or not).
So, this research is suggesting that maybe it’s the sarcopenia, the loss of muscle, and not the obesity that is contributing to increased mortality risk.
Another study published in 2014 looked at sarcopenia and mortality risk- but this study focused on hospitalized older adults. Researchers wanted to investigate the association between sarcopenia and risk of death during hospital stays (6).
Researchers found that those with sarcopenia were more likely to die during their hospital stay (6% of those with sarcopenia vs. 2% of those without sarcopenia died during their hospital stay).
They also found a significantly higher risk of death 1-year later (26% of those with sarcopenia vs. 14% of those without sarcopenia died within 1 year of their initial hospital stay).
It was concluded that sarcopenia was indeed associated with increased short- and long-term risk of death in hospitalized older adults (6).
Does this make sense? Sarcopenia appears to increase the risk of death regardless of BMI. And it is associated with higher rates of death when you get sick and go to the hospital. It is so important to maintain adequate muscle with aging.
Body Composition (Muscle vs. Fat Mass)
Let’s keep looking at this trend. In 2016 researchers sought to better understand the relationship between lean mass (muscle) and fat tissue in older adults. And more importantly, how they may be connected to all-cause mortality (7).
Researchers found that the more muscle older adults had, the lower the risk of all-cause mortality (death) and cardiovascular mortality. Interestingly those with the highest amount of fat mass did not have a significantly greater risk (7).
So, what does this mean? This research suggests that interventions in older adults should perhaps be focused on improving muscle mass instead of focusing on fat mass. [Preach!]
Yet another study published in 2016 concluded that fat-free mass index (AKA muscle) loss was related to an increased risk of death in older adults (8). And similar results have also been found in research done with frail, older adults (9).
So, let’s shift to look at frailty (weakness).
Frailty and Mortality

Whew! I know this is a lot of information and science, but it is important. Let’s keep going.
A 2017 study found that having a low level of body fat or having a pronounced decline in body fat is associated with an increased risk of mortality in frail older women (9).
I think it’s worth mentioning that this same study found that frail older women with a BMI between 25-34.6 had lower rates of mortality (10).
Yup. A BMI of up to 34.6, in the “obese” range, was associated with lower risk of death in older, frail women.
Researchers recommended that healthy BMI guidelines should be reevaluated for frail older women. We wholeheartedly agree.
I hope this continues to make sense. When there is less muscle, this increases frailty (weakness). It’s really the amount or percentage of muscle a person has and not the total weight.
Remember, earlier in the article when we looked at the illustration showing how a young person generally has more muscle than an older person? Older adults have less muscle than younger adults. When we compare BMI among young persons to older persons, it’s like comparing apples to oranges. It’s not the same.
This is likely why a higher BMI in the elderly is associated with lower rates of mortality. It’s more about the percentage of muscle when compared to fat. And this ties into sarcopenia, body composition, and frailty.
Health at Every Size and Older Adults
I do want to take a minute to address Health at Every Size®. This is a movement that says we shouldn’t focus on weight and we should really focus on quality of life and overall health. I am all for health at every size.
The question is, should we use weight as a focus in care of the elderly?
When I look at weight in older adults, I’m not looking at weight in terms of “are you too heavy” or “should you be losing weight”. I’m looking at opposite end. I’m concerned about the high risk of unintended weight loss and malnutrition in the older adult.
So, yes, I do think weight matters in the older adult. And that weighing the elderly is important to monitor for unintended weight loss.
I do recognize that getting weighed can trigger some individuals (ex. issues with body image, shame, triggering eating disorders, etc) and there will certainly be situations where it may not be appropriate to obtain weights.
But overall, I think we should be assessing weight in older adults. Let’s look at how.

Assessing Weight in the Elderly
OK, so we have learned that the BMI guidelines are different for older adults. We have learned that body composition and prevention of muscle loss has an important role in the heath of the older adult. So, what then are appropriate tools to use for assessing weight in the elderly?
We will be looking at usual body weight, the assessment of malnutrition, and the nutrition focused physical exam.
I want to reiterate that I am an advocate of weighing older adults to quickly identify and STOP unintended weight loss. However, not everyone needs regular weights.
Reasons not to weigh someone:
- History of eating disorders & weights can be triggering
- Unsafe to weigh (ex. they are a fall risk)
- They are on hospice & no longer want to be weighed
- They choose not to be weighed for any reason, it’s their own choice!
Usual Body Weight
BMI is “okay” to use for assessing body weight, as long as you are using a range appropriate for older adults. But an even better way to assess weight in the elderly is looking at usual body weight and weight stability.
No major gains and no major losses. This is important to remember. We need to focus on weight stability for the older adult. And preserving muscle mass.
Now let’s look at what the research tells us on weight stability in the older adult.
A research study investigated all-cause mortality and its association with weight, muscle, and fat mass in older men. Researchers found that older men who lost weight, muscle, or fat mass had a higher risk of mortality than men whose weight, muscle, or fat mass remained stable (12).
Another study found that weight cycling (losing weight then gaining it back- commonly known as “yo yo dieting”) and weight loss predicted impending mobility disability (read= loss of independence) and mortality (read= death) in old age (13).
Interestingly researchers found no risk of mobility disability or mortality with weight gain (13). Hmmm…. It’s all about that muscle. This study really underscored the importance of weight history.
This is why focusing on usual body weight and weight stability is so important in the elderly.
Identifying Malnutrition in the Elderly

In addition to monitoring for weight (and stopping unintended weight loss), it’s important to identify and address malnutrition early in the elderly.
In a nutshell, malnutrition is not getting the nutrition you need. This leads to a change in body composition (loss of muscle/fat) and loss of independence.
How do we identify malnutrition? There are several screening tools used in the older adult population to assess malnutrition. The Mini Nutrition Assessment (MNA) is the most widely accepted and validated nutrition screening tool for older adults regardless of where they live (14).
The MNA short form contains 6 questions looking at food intake decline, weight loss, mobility, psychological stress or acute disease, neuropsychological problems, and BMI (14). You’ll notice the MNA uses higher BMI ranges too.
You can access the MNA here.
A positive MNA screen should result in a referral to a geriatric dietitian.
Nutrition Focused Physical Exam
The last thing I wanted to talk about in this section is the nutrition focused physical exam. The nutrition focused physical exam is used by Registered Dietitian Nutritionists in the identification of malnutrition in older adults (15).
I won’t go into too much detail here, but the dietitian is looking at (15):
- Loss of muscle mass
- Loss of subcutaneous fat
- Fluid accumulation
- Grip strength
A dietitian can assess for malnutrition (and muscle loss!) even without weight, and certainly regardless of BMI. Because the most important piece of the puzzle does come down to muscle mass. Protecting muscle loss and stopping unintended weight loss is so very important in seniors.
Stopping Unintended Weight Loss

When looking weight loss, we need to look at the change in weight over time to determine if the weight loss is significant or severe loss. Although any loss of weight can be concerning.
The Centers for Medicare and Medicaid Services (CMS) defines significant unintended weight loss as a weight loss of (16):
- 5% body weight in 30 days, or
- 7.5% body weight in 90 days, or
- 10% body weight in 180 days
It should be noted that gradual weight loss over time (also known as “insidious weight loss”) is just as concerning (16). Obviously rapid muscle loss is concerning, but sometimes a slow loss can be easily missed.
You can learn more about this topic in my article on stopping unintended weight loss in older adults and weight loss in elderly must be stopped.
What if an Older Adult Wants to Lose Weight?
I hope by now you understand why BMI ranges are different in elderly and why it is important to focus on weight stability. But what is an older adult wants to lose weight?
An older adult may want to lose weight for a multitude of reasons. We live in a weight obsessed world. Sometimes the number on scale or the size on your clothes is more important to people than overall health.
Others may be told they must lose weight in order to have a procedure such as a knee replacement.
In those who want to lose weight or have a medical need, we need to make sure they are getting adequate protein and resistance training to preserve their muscle with weight loss. And they really should be working with a geriatric dietitian!
Research indicates there may be association between a distribution of protein throughout the day and higher muscle mass in older adults (17). So, make sure that good sources of dietary protein are consumed throughout the day. At breakfast, lunch, and dinner.
This is my final pearl of wisdom for you all- for older adults wanting to lose weight- first provide education. If they still want to lose weight, encourage protein and resistance exercise to maintain their lean body mass.
Preserve that muscle!
Summary
We covered a lot in this article. We discussed BMI in the elderly and went beyond to assessing weight and stopping unintended weight loss.
These were the key points I hope you remember long after reading this article:
- BMI guidelines are different for older adults
- Overall health is more important than BMI
- Usual body weight is the best way to “assess” weight in the elderly
- Unintended weight loss must be stopped
- Older adults who want to lose weight should work with a dietitian
Here’s to maintaining that muscle and to good health and independence with aging!
***To grab a free PDF version of this article click here.

References
- About Adult BMI. Centers for Disease Control and Prevention Website. https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. Reviewed April 10, 2020. Accessed May 17, 2020.
- Famularo P. Desirable body weight in the older adult: What does the current research indicate? Connections newsletter (Dietetics in Health Care Communities DPG); 2014; 40(1): 1-7.
- Winter JE, MacInnis RJ, Wattanapenpaiboon N, Nowson CA. BMI and all-cause mortality in older adults: a meta-analysis. Am J Clin Nutr. 2014;99:875-890.
- Walston, J. Sarcopenia in older adults. Curr Opin Rheumatol. 2012: 24(6):623-627.
- Batsis, J. A., et al. Sarcopenia, sarcopenic obesity and mortality in older adults: results from the National Health and Nutrition Examination Survey III. European journal of clinical nutrition. 2014:68(9): 1001-1007.
- Vetrano, Davide L., et al. Association of sarcopenia with short-and long-term mortality in older adults admitted to acute care wards: results from the CRIME study. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2014; 69(9): 1154-1161.
- Spahillari, A., et al. The association of lean and fat mass with all-cause mortality in older adults: The Cardiovascular Health Study. Nutrition, Metabolism and Cardiovascular Diseases. 2014; 26(11): 1039-1047.
- Graf, Christophe E., et al. Impact of body composition changes on risk of all-cause mortality in older adults. Clinical Nutrition. 2016; 35(6):1499-1505.
- Zaslavsky, Oleg, et al. Association of dynamics in lean and fat mass measures with mortality in frail older women. The journal of nutrition, health & aging. 2017; 21(1):112-119.
- Zaslavsky, Oleg, et al. Association Between Anthropometric Measures and Long‐Term Survival in Frail Older Women: Observations from the Women’s Health Initiative Study. Journal of the American Geriatrics Society. 2016; 64(2): 277-284.
- Jung, Hee‐Won, et al. Frailty status can predict further lean body mass decline in older adults. Journal of the American Geriatrics Society. 2014; 62(11): 2110-2117.
- Lee, Christine G., et al. Mortality risk in older men associated with changes in weight, lean mass, and fat mass. Journal of the American Geriatrics Society. 2011; 59(2): 233-240.
- Murphy, Rachel A., et al. Weight Change, Body Composition, and Risk of Mobility Disability and Mortality in Older Adults: A Population‐Based Cohort Study. Journal of the American Geriatrics Society. 2014; 62(8): 1476-1483.
- MNA Mini Nutritional Assessment. Nestle Nutrition Institute Website. https://www.mna-elderly.com/. Accessed May 17, 2020.
- White, J. V., P. Guenter, and G. Jensen. Characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet. 2012;112(5): 730-8.
- Niedert K, Dorner B. Nutrition Care of the Older Adult. Chicago, IL: Academy of Nutrition and Dietetics; 2016.
- Farsijani, Samaneh, et al. Relation between mealtime distribution of protein intake and lean mass loss in free-living older adults of the NuAge study. The American journal of clinical nutrition. 2016; 104(3): 694-703
ref: Hussain SM, Newman AB, Beilin LJ, Tonkin AM, Woods RL, Neumann JT, Nelson M, Carr PR, Reid CM, Owen A, Ball J. Associations of Change in Body Size With All-Cause and Cause-Specific Mortality Among Healthy Older Adults. JAMA network open. 2023 Apr 3;6(4):e237482-.

This article is very informative and well sourced. I do have one question. In my readings I’ve seen that doctors now say older adults should use their height before they began ‘shrinking’ for BMI calculations. Should that be applied to these guidelines when calculating BMI?
TIA!
Assessing height can be tricky for those who are unable to stand up straight or have spinal deformations. In those situations, we typically use alternative methods for obtaining height like arm span (where someone spreads their arms wide and we measure from fingertip to fingertip) and document it as “estimated height”. I think the big take-home message is that BMI is just one guideline. We’re most concerned with maintaining muscle mass and preventing unintended weight loss (which causes muscle loss). Hope this is helpful!
Hospice NP here. Somewhere along the line, I missed the memo about applicability of BMI with the elderly population. Great information with good references. I will be introducing to our team!
I’m so glad this was helpful! Thank you for the work that you do.
My mother, age 96, is trying to lose weight. She is 5’6″ and 180 pounds, so her BMI is already slightly under 30. Her plan for losing this weight is forgoing sugary sweet desserts at dinner every night and having a fresh fruit cup. I think if she looses 5-8 pounds that will be a good thing for her mobility and her morale. She walks quite a bit and attends a seated exercise class three times a week, so her muscles do get used. Although her appetite is still very good, she is obsessed with sweets, which are “empty calories.” With fewer sweets, she can apply her appetite to higher protein foods and foods with more nutrients. I think this is an example of a very old person who wants to lose some weight for good reasons. Thank you for your article, which is extremely helpful.
AMAZING ARTICLE! Something I have struggled with, especially being a younger RDN, is bringing the recent research and information into practice in my facilities. I was able to show this article to many members of the interdisciplinary team (many of them are older, so their practices are becoming outdated), and it changed so many of their outlooks on this. It was incredibly helpful that you also referenced the research behind everything. Definitely worth the read for all health professions.
Thank you! 🙂